Insurance Fraud Costs the U.S. $308.6 Billion Annually
Why is this study important? Insurance fraud is the crime we all pay for, whether through higher premiums,
law enforcement expenses, court costs, and in medical care. The actual cost of insurance fraud on American
citizens is impossible to measure accurately. This report seeks to use the best available data and resources to
accurately estimate the economic damage insurance fraud causes every year in our nation. It is intended to
inform consumers and to guide insurers, law enforcement, insurance regulators, and legislators in the need to
work together to protect consumers from insurance fraud crimes.
Why is the figure so high? In 1995 the Coalition Against Insurance Fraud announced an $80 billion estimate of
insurance fraud in America. That number became the most-cited insurance fraud statistic in the U.S. And while
the 1995 estimate addressed only property & casualty insurance, this report addresses all lines of insurance.
The 1995 estimate was also never updated or adjusted for inflation. Applying an inflation calculator alone
increases the $80 billion figure to $155 billion. The remaining additional $156 billion in estimated insurance
fraud includes the additional lines of insurance, notably healthcare, workers compensation, and life &
disability insurance. Also, in 1995 the internet was in its infancy. Today, the World Wide Web substantially
contributes to new forms of global insurance fraud that impacted the U.S. that did not previously exist.
How was this study conducted? The Coalition Against Insurance Fraud provides this study. When the decision
was made to do the first update in 27 years to the 1995 figure, the Coalition sought input and assistance from
key strategic partners who advised, peer-reviewed, and analyzed this report. These partners include the
International Association of Special Investigation Units, the National Insurance Crime Bureau, the American
Property & Casualty Insurance Association, and the Insurance Information Institute. To ensure a thorough and
independent report, all data collection, analysis, and the study document were prepared by the Colorado
State University Global White Collar Crime Task Force led by Dr. Michael Skiba. The team of PhD candidates at
CSU compiled data from the most reliable sources available for each line of insurance. Such sources include
the FBI, respected trade associations, and regulatory reporting filings. As the study notes, far better data
collection is needed by insurers and governmental agencies to better analyze and quantify the actual cost of
insurance fraud on the American economy.
For more information: Please refer to the Coalition Against Insurance Fraud website: www.insurancefraud.org
or contact the Coalition’s Executive Director Matthew J. Smith, Esq. via [email protected] or by
calling (202) 393-7332.

Study Conducted by:
Colorado State University Global
White Collar Crime Task Force
2022
In partnership with
THE IMPACT OF INSURANCE FRAUD ON
THE U.S. ECONOMY
A report from the Coalition Against Insurance Fraud

Contents
W W W . I N S U R A N C E F R A U D . O R G
I. INTRODUCTION OF THE STUDY
AND THE FRAUD PROBLEM ......................... 2
II. PREVIOUS $80 BILLION COST OF FRAUD
ESTIMATE EXPLAINED .................................. 3
III. METHODOLOGY OF STUDY ..................... 4
IV. SHORTCOMINGS AND
LIMITATIONS OF THE STUDY ....................... 5
V. INSURANCE FRAUD BY LINE OF BUSINESS
ANALYSIS ..................................................... 6
Property and Casualty Insurance Fraud. 6
Workers’ Compensation. 13
Premium Fraud. 19
Healthcare Fraud. 23
Medicare and Medicaid. 26
Life Insurance Fraud. 28
Disability Insurance Fraud. 31
Auto Theft. 33
V
I. COMPILATION OF THE LOB’S
INTO A FINAL 2022 COST ........................... 36
VII. STATEMENT ON AUTO THEFT ............... 37
VIII. RECOMMENDATIONS FOR
FUTURE STUDY ........................................... 37
X. APPENDIX ................................................ 38
XI. REFERENCES ........................................... 40
X. CONCLUSION .......................................... 38
OVERVIEW ................................................... 1
ACKNOWLEDGMENTS ................................. 41
OVERVIEW
The Coalition Against Insurance Fraud was created in 1993 and remains the nation’s only
consumer advocacy organization devoted to educating and protecting American citizens
from the cost and damage of insurance fraud. The Coalition consists of more than 260
organizations committed to the fight against insurance fraud. These organizations include
federal and state agencies, insurance regulators, legislative and insurance trade
associations, state attorneys general, prosecutors, law enforcement agencies, the majority
of America’s leading insurance carriers across all lines of insurance, and select companies
and law firms assisting in fighting insurance fraud.
In approximately 1995, the Coalition released an estimate of the cost of insurance fraud in
the United States as being $80 billion every year. Unlike other large economic figures, such
as the national debt, the estimate of the cost of insurance fraud is an annualized number,
meaning the financial counter resets at zero and begins anew every January 1st. The $80
billion impact for many years has remained the most often cited insurance fraud statistic
across the nation. Released 27 years ago, the figure has not been updated nor adjusted for
inflation or the advent of new forms of insurance fraud. The time has come to both update
and provide more substantial support for a new defined cost of insurance fraud that
accurately reflects the United States in the 2nd decade of this new millennium.
The Coalition extends its deepest appreciation for the support and contribution of our
partners in this study: the International Association of Special Insurance
Investigators, the American Property & Casualty Insurance Association, the
National Insurance Crime Bureau, and the Insurance Information Institute. This
study also would not have been possible without the support of our members who
support the work done by the Coalition every day. Finally, credit for the work behind this
study goes fully to Dr. Michael Skiba and the research team at the Colorado State
University Global White Collar Crime Task Force. We commend their tireless dedication,
hard work, and excellent analysis upon which this study is firmly based.

2
I. Introduction to the Study and the Fraud Problem
Insurance fraud is one of the most costly and damaging forms of fraud crimes in the
United States and globally. Fraud takes many forms; as scammers change their
methods daily to find new gaps and vulnerabilities. Insurance fraud results in monetary
damage but also causes humanitarian harm. In the area of medical fraud, patients are
often put at great risk and subjected to unnecessary treatments and procedures as a
result of unscrupulous providers attempting to inflate medical billing charges. Thus,
insurance fraud is widespread and has a dangerous impact on our society as a whole.
The purpose of this study is to develop a new cost estimate of the economic impact of
insurance fraud in the United States. Being released in 2022, the estimate represents
the current state of fraud and is intended to assist policymakers, companies, agencies,
government entities, and the public to gain a clearer understanding of the true nature
and scope of the insurance fraud problem. There are no prior studies that have
focused on this level of depth in developing a cost estimate of insurance fraud,
therefore this research endeavor is a truly ground-breaking project. Having a current
cost estimate will undoubtedly assist with creating increased awareness of the fraud
problem which will aid the allocation of resources for more highly focused counter-
fraud strategies.
Colorado State University Global’s White Collar Crime Task Force (WCCTF) is the
research arm spearheading this study, working on behalf of the Coalition Against
Insurance Fraud. The Coalition appreciates the support and assistance of our partners
in this study, the International Association of Special Investigation Units (IASIU), the
American Property & Casualty Insurance Association (APCIA), the National Insurance
Crime Bureau (NICB) and the Insurance Information Institute (III). Many other insurance
carriers, government agencies, non-profit organizations, industry groups, and
individual fraud fighters have all assisted with the development of this project. The
WCCTF consists of dozens of CSUG staff, Ph.D. faculty, researchers, and assistants,
but the primary lead investigators for the purposes of this study were Dr. Greg Koehle,
Landon Palmer, and Allison Blackburn.
This research publication will consist of the following sections:
I. Introduction of the study and the insurance fraud problem.
II. Previous $80 billion cost of fraud estimate explained.
III. Methodology of the study.
IV. Shortcomings and limitations of the study.

3
V. Line of business (LOB) analysis.
a. Current and existing research on the cost of fraud of specific LOBs.
b. Research calculations on the updated cost for the specific LOBs.
c. Compilation of the LOBs into a final 2022 cost estimate
VI. Statement on auto theft.
VII. Recommendations for future studies.
VIII. Conclusion.
IX. Appendix.
X. References.
II. Explanation of the Previous $80 Billion Cost of
Fraud Estimate
The Coalition circulates an estimate of the current cost of fraud as $80 billion annually,
which is the most widely used and popular statistic on insurance fraud cited in multiple
channels daily. Many industry professionals opine that this number is an incredibly
conservative figure and thus the inception of this 2022 study was to develop an entirely
new and up-to-date cost of insurance fraud in the United States. The Coalition
estimates that the $80 billion figure was developed in or around 1995. As a basic first
step in estimating a new cost of fraud, the WCCTF started with the baseline of $80
billion in 1995 and converted that amount into “present-day” dollars.
Using a standard Consumer Price Index (CPI) conversion of $80 billion in 1995 to
January 2022 results in an 81.5% inflation rate, which would convert into a 2022 cost
of fraud in the United States at $145 billion! It is the goal of the WCCTF and this study
to compile a new statistic in a highly methodological manner to present an accurate
2022 cost of insurance fraud.

4
III. Methodology
The WCCTF considered multiple methodological approaches as the foundation of this
study. Consideration was made to conduct the research using a quantitative
methodology, which would involve developing a research instrument in the form of a
survey, which would then be circulated in the insurance industry. The benefit of this
methodology would be real-time results directly from the industry. The WCCTF
explored this option but discovered that this approach would be problematic due to
data privacy concerns. Due to privacy issues with the release of claims, policy, and
fraud information, gathering specific data from carriers and industry groups via a
survey would be incredibly challenging, and yield sub-par data sets. After contacting
several carriers which had data set sources, it was clearly understood by the WCCTF
that the carriers were very resistant to releasing any data outside of their respective
corporate environments, thus making this quantitative methodology, not a viable
research option.
A qualitative methodology was also considered, whereby the researchers would
perform in-depth interviews with industry professionals on fraud cost and
measurement. This would be a very beneficial approach as direct contact and
feedback would be gathered. However, the WCCTF realized that this approach would
also result in the same data and information privacy challenges and therefore would
not be an ideal structure for this research endeavor.
The WCCTF pondered many other research approaches and considered those options
along with the timeframe and resources for this study and thought using available data
sets would be the best option. The WCCTF conducted initial exploratory searches for
several months for available data and existing research on insurance fraud and realized
that there are many data sets, studies, and publications that have already been
performed that can be utilized as the core data points for this current study. Therefore,
the WCCTF decided that the structure of this study will consist of locating, reviewing,
and analyzing currently available research and data sources, in other words, the
WCCTF will not be collecting any “new” data as part of this study.
In each of the Line of Business (LOB) sections, the WCCTF will address the reasoning
behind the choice to utilize specific data as connected to that line of business. The
WCCTF considered and reviewed hundreds of sources to serve this study, but the final
data was chosen based on those sources that were aligned with organizations that had
the highest degree of creditability in the industry and used the most accurate and
effective method of data collection.

5
The WCCTF searched for data within five years of this study date (2016 or newer) to
accurately represent the most current state of the insurance problem. This five-year
range provides robust data as it includes pre-covid data (2016-2020) and covid data
(2020-present). When data was used that was considered somewhat “dated,” the
WCCTF extrapolated the data and metrics and applied a CPI conversion to reflect
today’s cost. This CPI conversion will be explained in detail within the appropriate
sections of the study where it was utilized.
The next phase of the preparation was to identify the lines of business that would be
included in the cost of insurance fraud analysis. After lengthy discussions with the
Coalition and other stakeholders, it was determined that this study would focus on the
following lines of business:
1) Property and Casualty
2) Workers’ Compensation
3) Premium Fraud
4) Healthcare
5) Medicare and Medicaid
6) Life Insurance
7) Disability Insurance
8) Auto Theft
IV. Shortcomings and Limitations of the Study
The WCCTF will be using existing research and data as the core elements of this study,
and accordingly, as with any credible research, there are limitations and shortcomings.
Considering that existing data is being used, the research results are therefore limited
in certain areas as this research was already gathered under pre-set parameters.
Therefore, the team cannot act fluidly and alter data gathering parameters as the study
unfolds, the team must analyze the data that was already captured, which presents
inference and results limitations. However, even with these shortcomings and
limitations, the research team is confident that the results will be credible, sound, and
provide an accurate picture of the current cost of fraud in the United States.
Compiling one cost of insurance fraud for the entire insurance industry across multiple
LOB’s will create a new and fresh picture of the state of insurance fraud. However, it is
understood that each specific insurance company, insurance-related organization,
government agency, industry group, etc. has its own unique place in the insurance
industry. Thus, due to the many unique organizations that exist, certain sections and
LOB’s of this study may not be applicable. It is recommended that insurance
organizations use this study as a baseline and then if needed, modify the findings
revealed in this study to their unique situations.
6
V. Insurance Fraud by Line of Business Analysis
Property and Casualty Insurance Fraud
a) Introduction to the problem:
Property and casualty insurance is defined as a type of insurance that provides
protection for two main areas. First, it protects items that the insured owns. Secondly,
it provides liability coverage as protection for an insured if the insured is found culpable
in an accident and causes property damage or personal injury to another person.
Property insurance is referred to as a “first-party” coverage in that it provides for losses
related to a policyholder’s property, whereas casualty, or liability, insurance is referred
to as a “third-party” coverage, implying it protects a policyholder against the claims of
others. Property and casualty insurance can be written to apply to automobiles,
homes, and businesses. There are three basic types of property loss: 1) loss of or
damage to the article itself, 2) loss of income from the use of the article, and 3) any
extra expense incurred due to the loss of the article. Casualty insurance, which covers
liability losses, are losses that occur as a result of the insured’s interactions with others
or their property. To be liable, the individual must be guilty of negligence or the failure
to use proper care. There are generally three types of liability insurance: 1) general
liability, 2) professional liability, and 3) product liability.
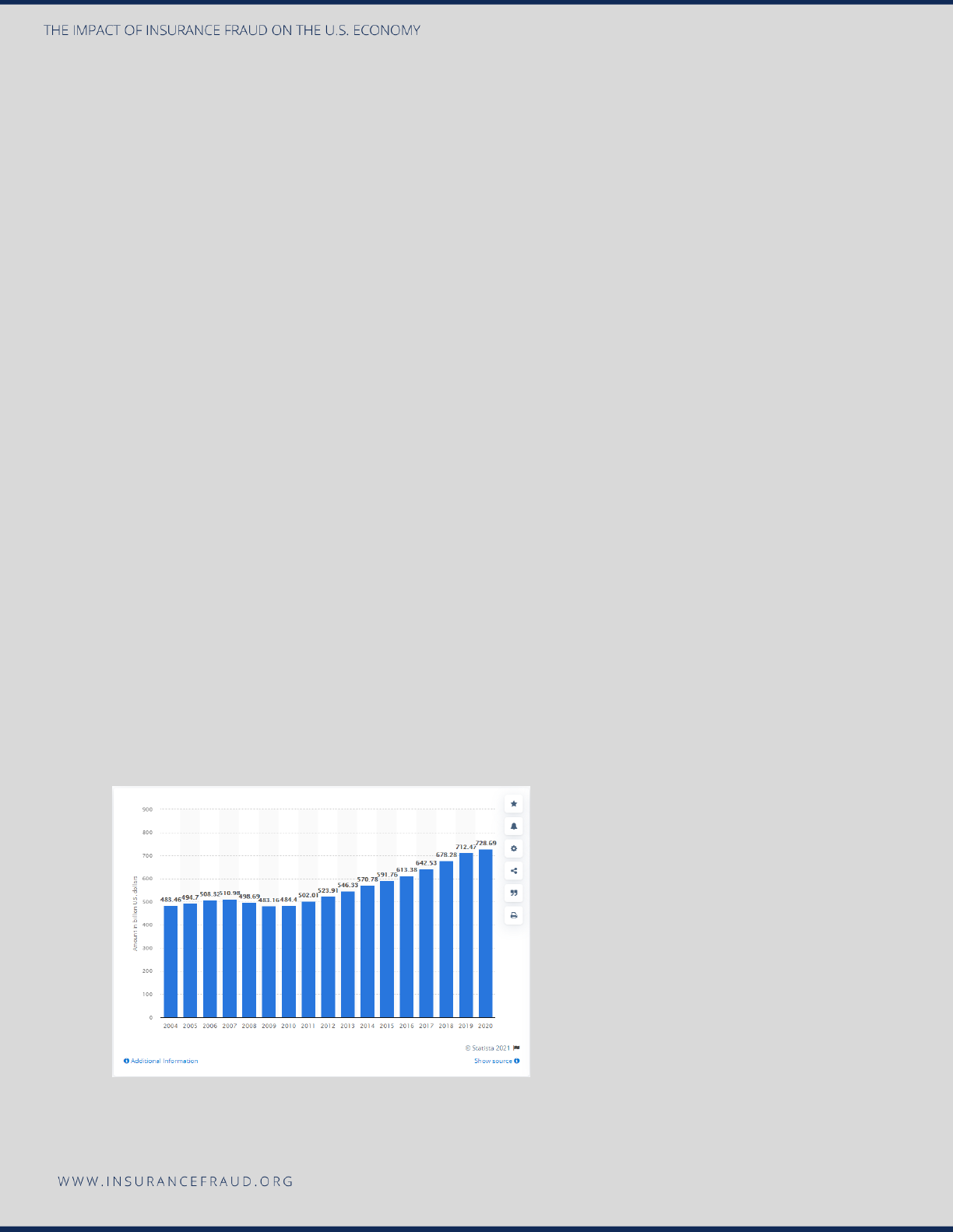
The following three visuals reveal interesting statistics on the property and casualty
industry in the United States.
The following graph shows direct premiums of property and casualty insurance in the
United States from 2004 to 2020 (in billion U.S. dollars).
Source: Statista 2021
7
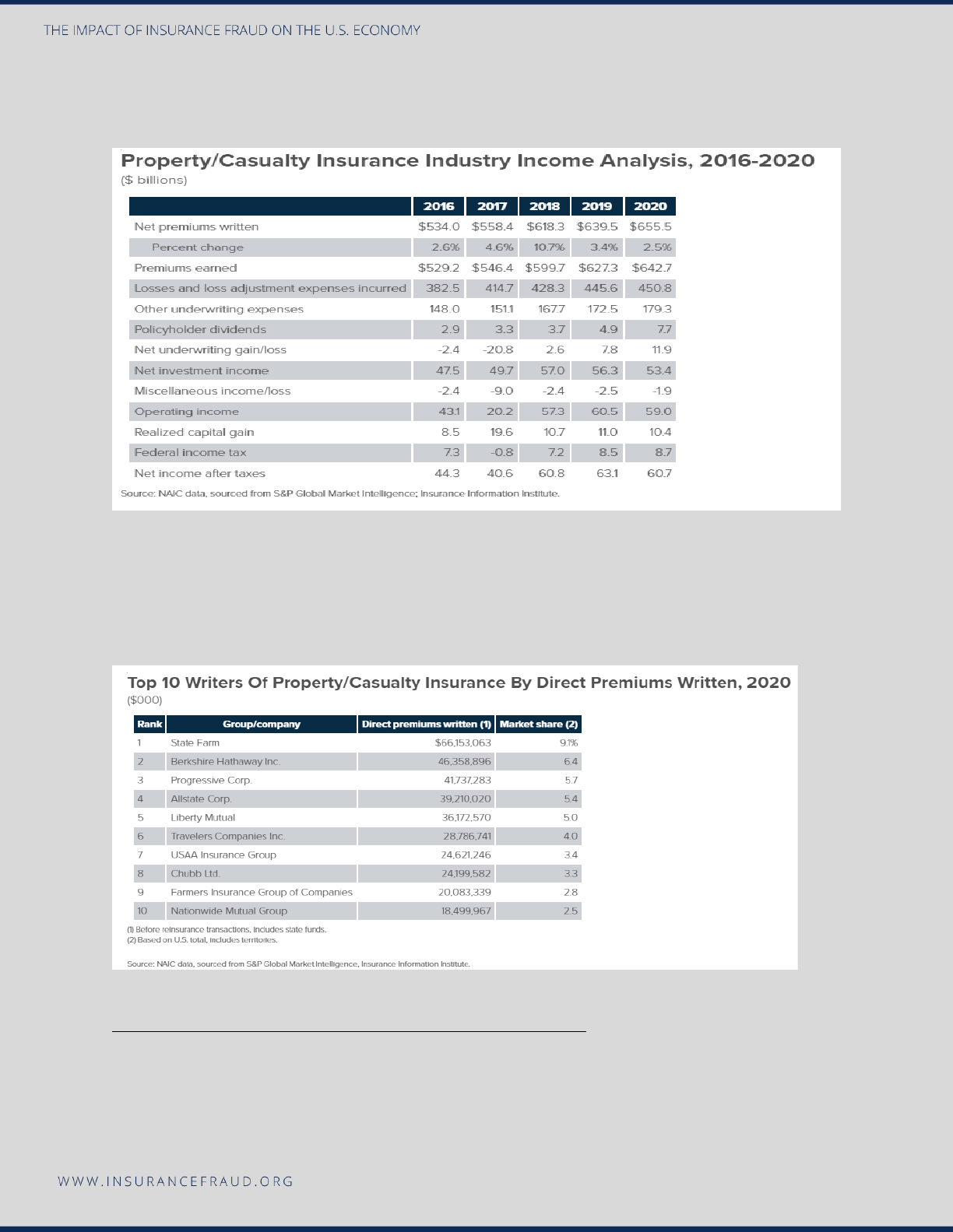
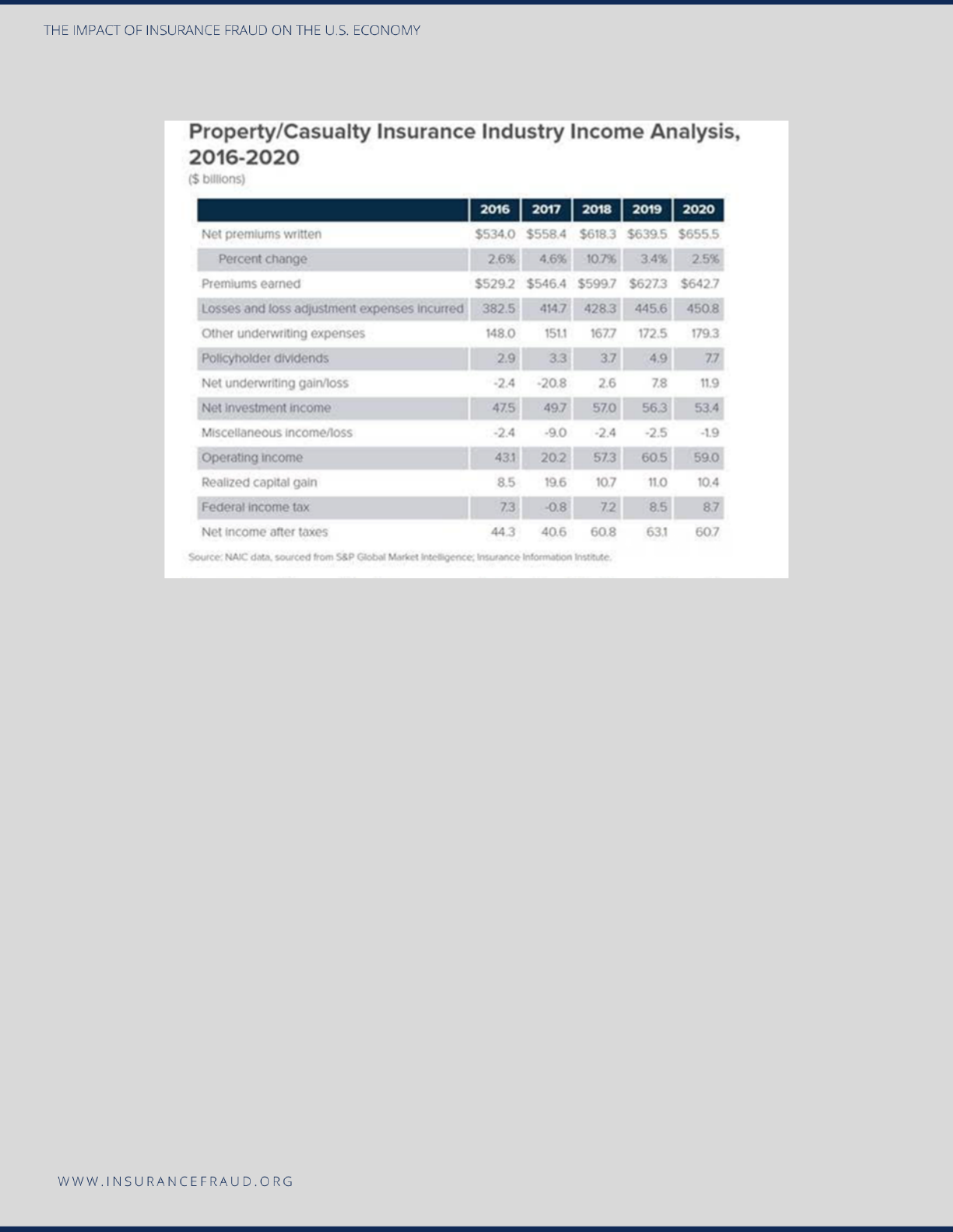
The following table shows a high-level property and casualty insurance industry
income analysis of 2016-2020 in billion U.S. dollars.
Source: Insurance Information Institute. (2021). Facts + Statistics: Industry overview.
https://www.iii.org/fact-statistic/facts-statistics-industry-overview
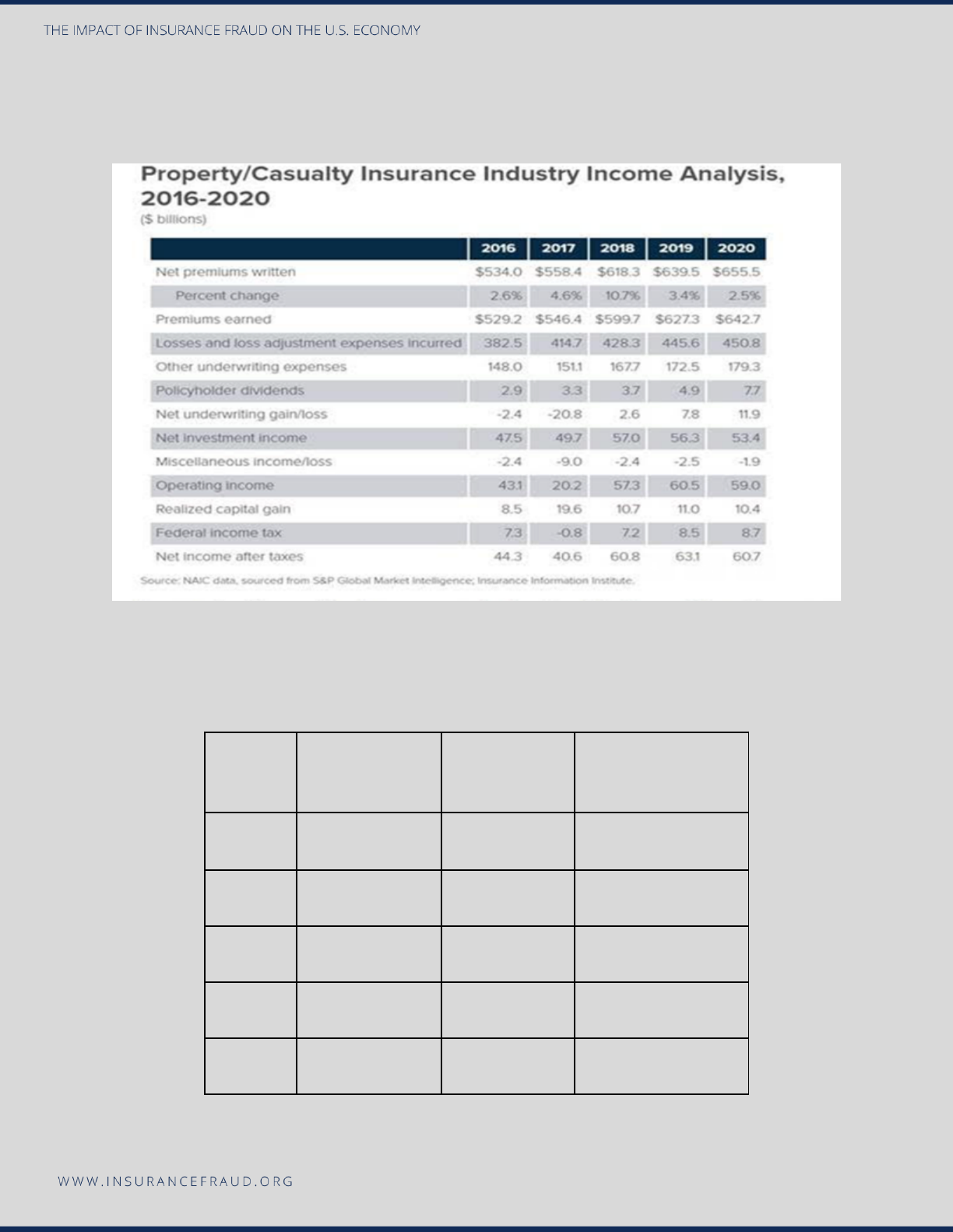
The following table shows the direct written premiums of the top 10 property and
casualty carriers in the U.S. in billion U.S. dollars.
Source: Insurance Information Institute. (2021). Facts + Statistics: Industry overview.
https://www.iii.org/fact-statistic/facts-statistics-industry-overview
b) Existing data pertaining to property and casualty fraud costs.

8
In addressing the current cost of fraud in the property and casualty line of business,
multiple sources were considered to assist with locating a new monetary amount.
Considering the structure of this study was one whereby the research team was not
gathering new data through qualitative or quantitative methods, an extensive search
was performed to secure as many potential sources of existing data and monetary
estimates on the cost of property and casualty fraud that have already been
performed. The research indicated that there is inconsistency with the definition of
what specific lines of business are included in property and casualty insurance.
Therefore, to provide an accurate metric on the current cost of property and casualty
fraud, the research team took great effort in clearly investigating what specific lines of
business were used in any research study or publication that helped calculate the
current cost. This was done to ensure that there was not an overlap in lines of business
that would potentially skew the final data.
Accordingly, there were two lines of business that are oftentimes included in property-
casualty fraud; auto theft and workers’ compensation. For purposes of this study,
those two lines of business will be analyzed separately to create a more accurate and
precise final figure on the cost of fraud. The research team removed those two lines of
business from this property and casualty cost and will focus on those separately to
provide a more accurate metric.
Auto theft is a type of fraud that is traditionally included in property and casualty fraud
and for the purposes of this study, the research team decided to analyze auto and
home theft as an entirely separate line of business. Therefore, there will be no auto and
home theft statistics included in this cost estimate for property and casualty fraud.
Workers’ compensation fraud is sometimes included in property and casualty fraud;
however, for the purposes of this study, the research team focused on workers’
compensation as an entirely separate line of business. Therefore, there will be no
workers’ compensation cost included in this property and casualty metric.
Regarding existing research and cost estimates for property and casualty fraud,
several sources were identified. The Federal Bureau of Investigations (n.d.) estimates
that insurance fraud (non-health) is estimated at more than $40 billion annually. *The
Insurance Information Institute (III.org) makes the following statement on its website:
“In the late 1980s, the Insurance Information Institute interviewed claims adjusters and
concluded that fraud accounted for about 10 percent of the property/casualty (PC)
insurance industry’s incurred losses and loss adjustment expenses each year. Using
that measure, in 2019 and 2020 P/C fraud would amount to $38 billion each year. The
figure can fluctuate based on line of business, economic conditions, and other
factors.”
9
*The III did not specify exactly how they derived at this figure, but the WCCTF
estimates that they first took 2019 and 2020 incurred losses (Loss & LAE) and then
multiplied that figure by 10% (average percentage claim fraud). The chart below is a
visual representation of how the WCCTF believes they arrived at the $38 billion figure.
As quoted by the III (above) they explain that they used the 10% average percentage
claim fraud as it was based on a study that they performed in 1980 by interviewing
claim adjusters from the industry. The WCCTF found that the 10% the III utilized for the
percentage of fraud in claims was also consistent with independent private
consultation research studies the WCCTF has performed and is also a percentage that
is widely cited as credible by many leading anti-fraud organizations, such as the ACFE,
and the Coalition; thus, the WCCTF deemed 10% as a credible percentage to use as
the average percentage of fraud in claims as a basis for this current 2022 study.
Casualty fraud, which is a component of property and casualty fraud, was studied in
2015 by the Insurance Research Council (2015) which estimated that casualty fraud
accounted for between 15% and 17% of total claims payments for auto insurance
bodily injury in 2012. The study estimated that between $5.6 billion and $7.7 billion
was fraudulently added to paid claims for auto insurance bodily injury payments in
2012. Using a standard formula CPI index and adjusting for inflation, the new cost of
casualty fraud in current dollars would be estimated between $6.8 and $9.3 billion. All
of the data and figures that resulted from the previously stated analysis will be used as
a baseline as the study unfolds.
*The $40 billion statistics from the FBI was deemed one of the most credible to
estimate insurance fraud as they are one of the premier law enforcement agencies in
the world and accordingly maintain a robust research platform and have a vast network
to gather credible and accurate data. The WCCTF located research by several state
Year
Loss &
LAE
Fraud
(10%)
Incurred
Losses*
Fraud (IL)*
2016
382.5
38.25
323.595
32.3595
2017
414.7
41.47
350.8362
35.08362
2018
428.3
42.83
362.3418
36.23418
2019
445.6
44.56
376.9776
37.69776
2020
450.8
45.08
381.3768
38.13768

10
insurance organizations, but due to the fact that this research was not available
consistently for every state, this was deemed as an unviable source.
*The Insurance Information Institute was chosen as the second most reliable, credible,
and effective data source as the III is one of the most well-respected members of the
insurance industry. Since 1960, the III has been one of the most trusted sources of
data for consumers, the media, and professionals in the insurance industry and at its
core organizational function researches and publishes information, statistics, and data
on the insurance industry.
*The 2012 study that the Insurance Research Council performed was chosen as the
primary data source as the IRC has been providing the property and casualty industry
with robust research since its inception in 1977, and along with the III is considered
one of the top insurance research organizations. The WCCTF found little to no studies
specifically focused on casualty fraud and therefore this somewhat dated 2012 study
by the IRC was seen as the most effective data source for the purposes of this study.
c) Research teams’ calculation on the updated cost of property and casualty
fraud.
The WCCTF considered the results developed in section b above but also wanted to
explore opportunities to develop an entirely new metric. Regarding a reasonable
methodology to calculate the current cost of property and casualty fraud, the WCCTF
concluded that an accurate formula would be to begin with the Loss Adjustment
Expense (LAE) for each year and then extract 10% of that LAE figure to arrive at a new
estimated cost of property and casualty fraud. The Actuarial Standards Board (2022)
defines the Loss Adjustment Expense as the “cost of investigating, administering,
determining coverage for, settling, or defending claims even if it is ultimately
determined that the claim is invalid.” It is also known as “claims adjustment expense.”
Accordingly, the WCCTF utilized the LAE as circulated by the III (Insurance Information
Institute, 2021, Facts + Statistics: Industry overview) and then calculated the new cost
of fraud by multiplying LAE by 10%.
Figure 1 shows a visual of the 2016-2020 property and casualty industry metrics for the
U.S. The LAE that is the focus of this analysis is seen in the 4
th
row, titled: “Losses and
loss adjustment expense incurred.”
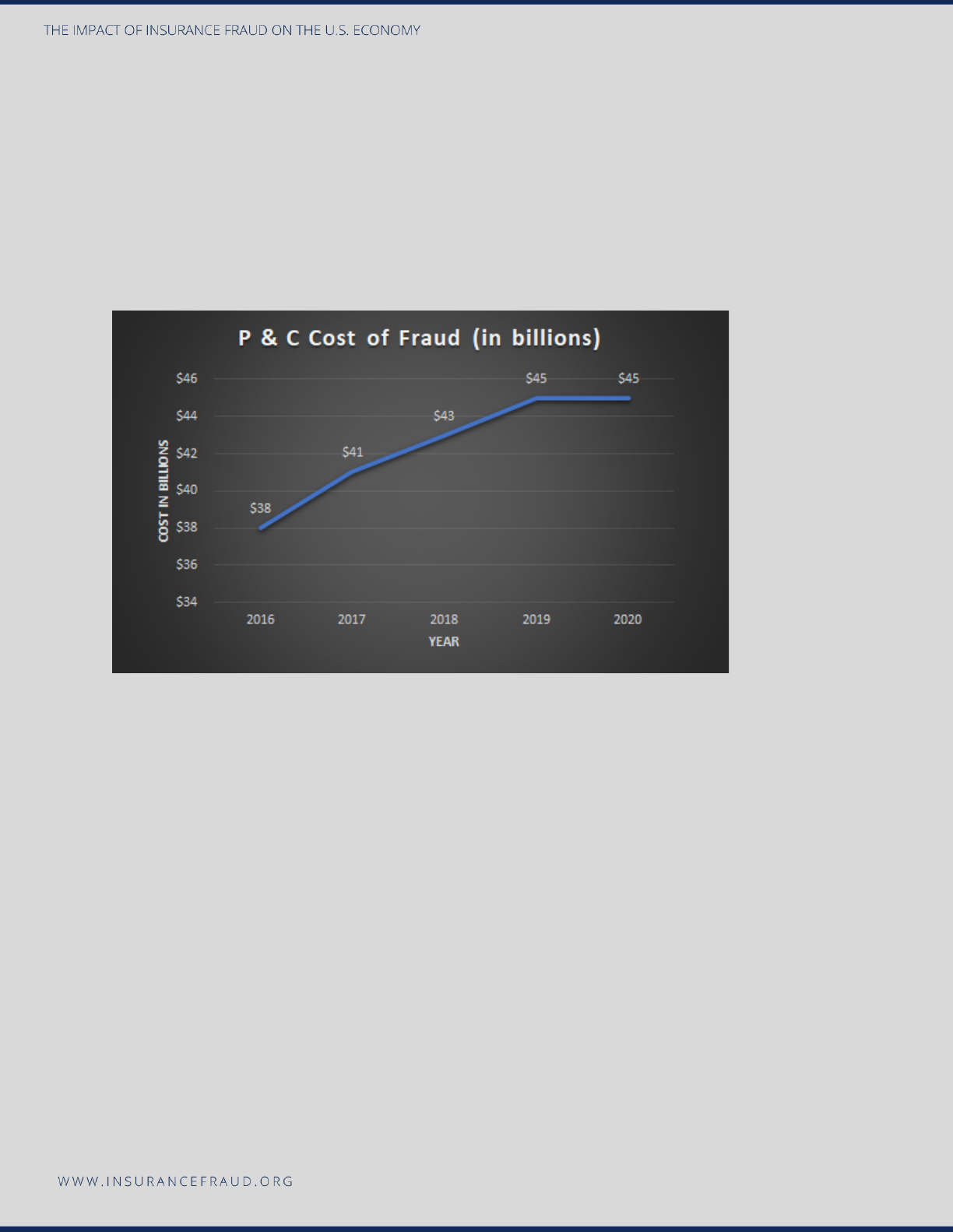
The final cost of property and casualty fraud was assessed from 2016 to 2020 by using
the LAE for each year and then multiplying that number by 10%. The results can be
viewed in two formats in Figures 2 and 3.
11
Figure 1
Source: Insurance Information Institute. (2021). Facts + Statistics: Industry overview.
https://www.iii.org/fact-statistic/facts-statistics-industry-overview
Figure 2: Cost of Property and Casualty Fraud 2016-2020 (in table format).
YEAR
LAE (in billions)
FRAUD (10%)
COST (in billions)
2020
450.8
10%
$45
2019
445.6
10%
$45
2018
428.3
10%
$43
2017
414.7
10%
$41
2016
382.5
10%
$38
12
Figure 3: Cost of Property and Casualty Fraud 2016-2020 (in graph format).
In conclusion, as indicated in a visual format in Figures 2 and 3 above, the WCCTF
estimates that the current cost of property and casualty fraud in the United States is
$45 Billion. When we consider the costs as revealed in section b from the FBI ($40
billion), III ($38 billion), and the IRC (between $5.6 and $7.7 in casualty fraud), the
current estimate of $45 billion appears credible and reliable.
Statement of No-fault
No fault insurance is required in twelve US states: Delaware, Florida, Hawaii, Kansas,
Massachusetts, Michigan, Minnesota, New Jersey, New York, North Dakota, Oregon,
and Utah. In addition, no-fault policies are optional, but can be purchased in seven
other states: Arkansas, Kentucky, Maryland, South Dakota, Texas, Virginia,
Washington, and the District of Columbia.
There is no doubt that fraud exists in claims submitted under no-fault coverage,
whether in the form of staged accidents, medical provider fraud, or other schemes,
there is significant fraud exposure and the potential for serious financial loss. During
the initial data research phase of this study, it became immediately apparent to the
CSUG team that there is an overall lack of distinct reporting and recording of no-fault
insurance fraud in the United States. Most no-fault states include no-fault fraud as part
of their property and casualty metric, however, no-fault is not specifically defined and
calculated as a separate line item in that property and casualty metric in almost all
instances. Therefore, given the structure of the method that organizations currently

13
record and report fraud, and specifically how there is a lack of specific fraud recording
of no-fault fraud, it is not possible to develop a separate cost of no-fault insurance
fraud in the United States. However, it may be safely assumed that no-fault fraud is
included as part of the property and casualty final cost.
One of this study's key take-aways and recommendations is that no-fault states
specifically define and record no-fault insurance fraud as an entirely separate form of
fraud. Having an accurate and separate measurement of no-fault fraud will provide
insights into the cost of fraud that is ultimately passed on to the consumer.
Statement of the property and casualty metric.
The goal of this study is to increase awareness of the insurance fraud problem by
circulating a new and impactful cost of fraud and also serve as a starting point to
create specific calls to action for all involved in anti-fraud efforts to take additional
steps to modify and enhance our existing fraud reporting. As identified in the
“Statement of No-Fault” text above, there are significant gaps in the reporting of
property and casualty fraud. During all phases of research and data gathering in
regards to property and casualty fraud, it was extremely challenging to determine what
specific data was gathered when the research team located a data source. In almost all
of the instances, the term “property and casualty” was used very regularly in data
sources and articles, but there was never any specific breakdown of what specific
coverages were included. These gaps in reporting are significant opportunity areas for
the insurance industry to develop new protocols. As stated earlier, no-fault fraud needs
an entirely separate line item for reporting and the same is true for all forms of auto
insurance fraud. Most carriers and states capture auto insurance fraud as part of their
property and casualty measurement, and accordingly, auto insurance fraud is included
in the present study under the property and casualty figure. This study has identified a
significant gap in reporting related to auto insurance fraud; the research team
recommends that companies and states specifically define what exactly is included in
their definition of property and casualty statistics and record and report by the type of
coverage, such as no-fault (1st party coverage), auto property and casualty, fire
property and casualty, casualty (3rd party), etc… as this will provide deeper insights
into the impact of each specific area.
Workers’ Compensation
a) Introduction to the problem:
Workers' compensation insurance is accident coverage that is paid by employers. If an
employee is injured on the job, the employee may receive benefits to cover medical
bills, rehabilitation costs, and lost wages. Some policies even provide a death benefit.

14
Workers’ compensation insurance only applies if the employee is injured while
performing the duties of the actual job. Workers’ compensation systems vary from
state to state, thus there are many different systems in place in the United States,
creating challenges in regard to measurement, research, and collaboration.
Workers’ compensation fraud is defined as “a completely fabricated injury, or a
legitimate injury that is exaggerated by an employee to claim additional money.” There
are many legal definitions of workers’ compensation fraud, but the most widely used
definition (Insurance Council of Texas, 2022) states:
“Workers’ compensation fraud occurs when someone willfully makes a false statement
or conceals information in order to receive workers’ compensation benefits or prevents
someone from receiving benefits to which they might be entitled.”
Some examples of workers’ compensation schemes may include, overstating injuries
or limitations, concealing records that could be detrimental to a claim, claiming an
injury sustained on the job when it occurred elsewhere, and working “under the table”
while collecting temporary disability benefits.
One of the most challenging aspects of workers’ compensation fraud is that it is not
considered a high-profile crime; most individuals are not even aware that workers’
compensation scams are even a crime. Fraudulent workers’ compensation claims are
very damaging to businesses as they create a negative impact on a company’s bottom
line, revenue, and culture. Workers’ compensation fraud is not limited to employees,
there is also a significant amount of fraud that occurs from employers themselves in
the form of misclassifying workers and other policy misrepresentations to reduce the
premium amount that the employer actually pays to the insurer. Medical provider fraud
is the third area of fraud in workers’ compensation. This occurs when unscrupulous
medical providers overbill and bill for services not rendered.
According to the Bureau of Labor Statistics (2022), it costs employers an average of
$957 per year per worker to provide legally required workers' compensation coverage,
which accounts for about 1.2 % of the total average employee compensation costs
incurred by employers. The average cost is $915 per worker in the private sector and
$1,186 per worker in state and local governments. When we look at the disturbing
trajectory of fraud in workers’ compensation, we also see an emerging, highly
disturbing pattern. As an example, Texas reported 99,850 workers’ compensation
claims in 2020, a significant increase from 73,628 in 2019 (Texas Department of
Insurance, 2022).
15
There are instances when a company feels justified to issue a workers’ compensation
denial. Research shows (Business Insurance, 2018) that claim denial rates increased
from 5.8% to 6.9% between 2013 and 2017.
The top 10 most common reasons for claim denial were:
● No medical evidence of injury.
● No injury per statutory definition.
● Reservation of rights, which is an insurer’s notification to an insured that
coverage for a claim may not apply.
● Pre-existing condition.
● Idiopathic condition
● Intoxication or drug-related violation.
● Non-work-related stress.
● Failure to report an accident promptly.
● The injured person doesn’t meet the statutory definition of an employee.
● Misrepresentation.
Below are several interesting visuals on workers’ compensation insurance as published
by the Insurance Information Institute (III). These provide some framework for this
challenging line of business.
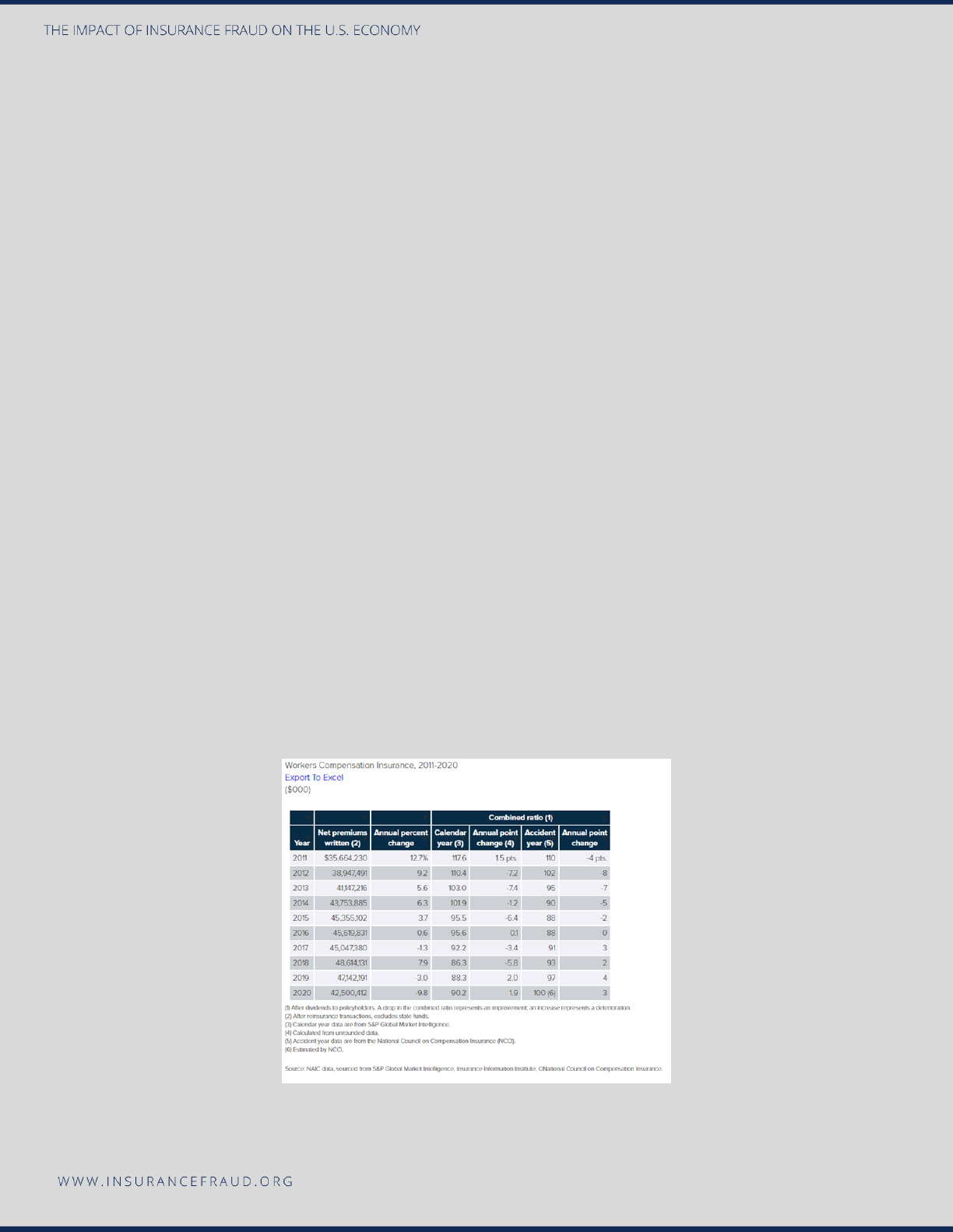
Figure 4 below shows interesting statistics on workers’ compensation insurance dating from 2011-2020.
It is interesting to note the pivot point starting in 2019 when the Net Written Premiums began to decline
from a steady growth since 2011.
16
Source: Insurance Information Institute. (2021). Facts + Statistics: Workplace Safety/Workers Comp.
https://www.iii.org/fact-statistic/facts-statistics-workplace-safety-workers-comp
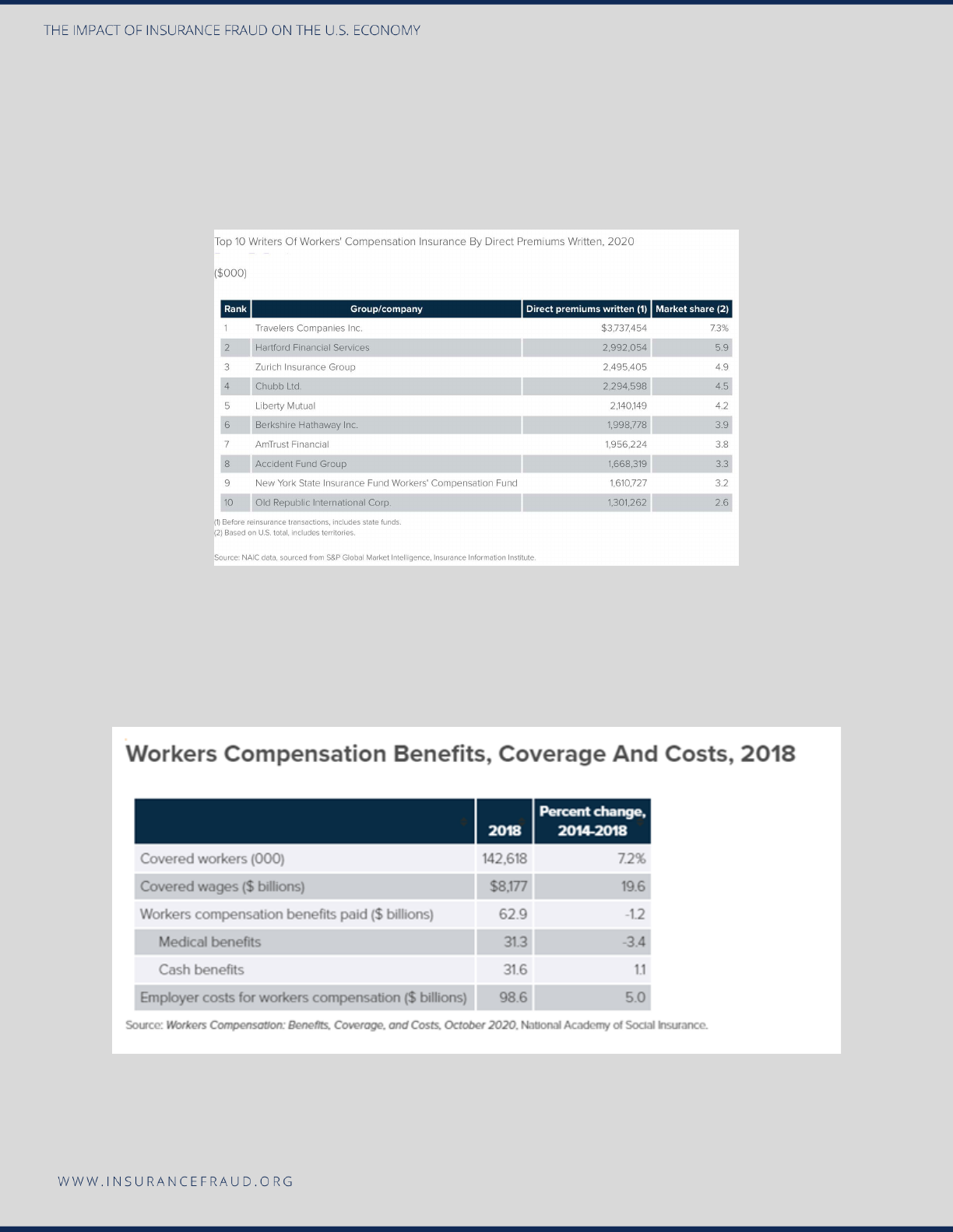
Figure 5 below shows the 2020 top 10 workers’ compensation insurance carriers by Direct Premiums
Written. As seen below, these 10 carriers comprised 43.6% of the entire market share of workers’
compensation premiums.
Source: Insurance Information Institute. (2021). Facts + Statistics: Workplace Safety/Workers Comp.
https://www.iii.org/fact-statistic/facts-statistics-workplace-safety-workers-comp
Figure 6 below shows the coverage and costs of workers compensation benefits in 2018. This chart
provides a nice indicator of the significant money that is involved in this type of coverage.
Source: Insurance Information Institute. (2021). Facts + Statistics: Workplace Safety/Workers Comp.
https://www.iii.org/fact-statistic/facts-statistics-workplace-safety-workers-comp
17
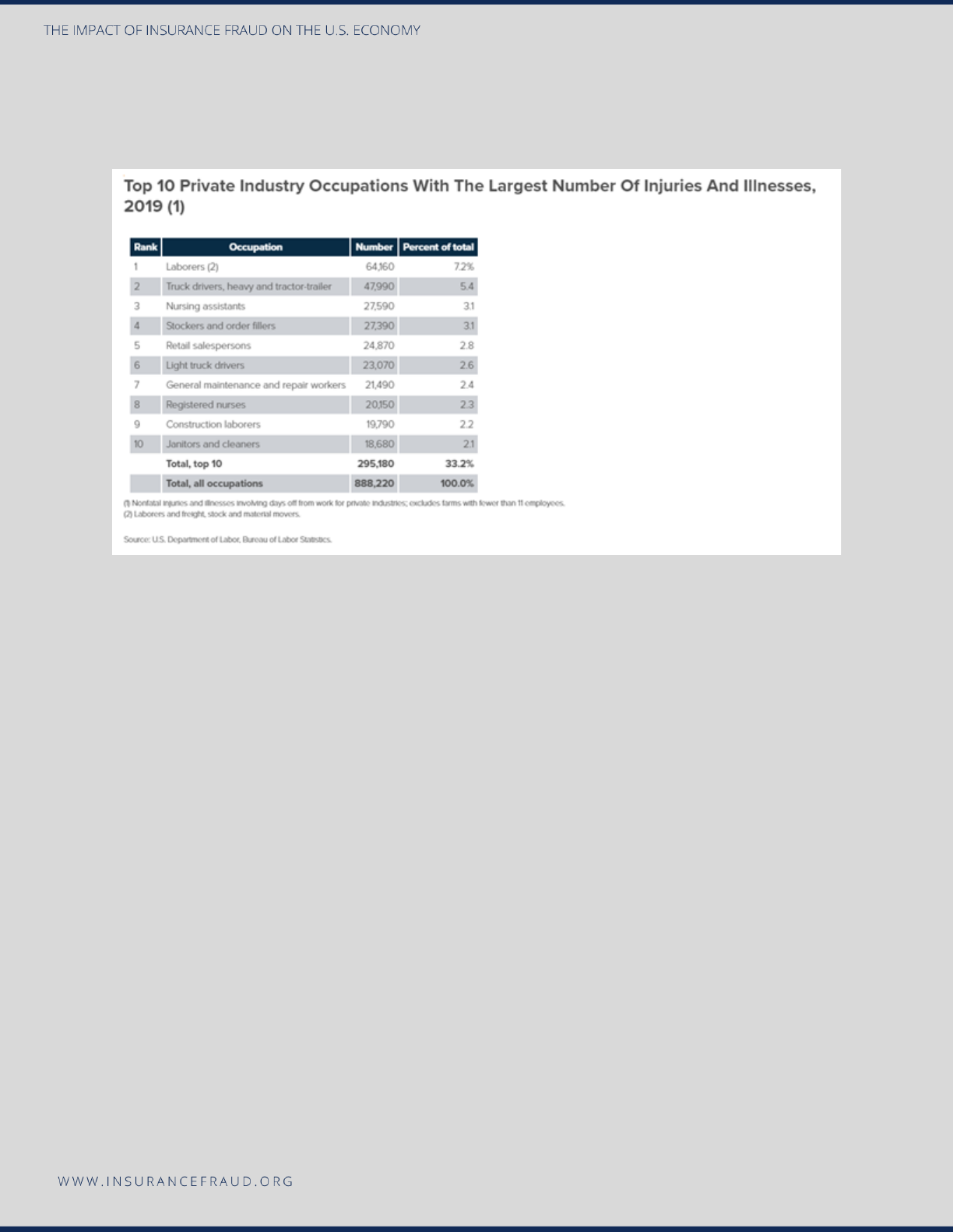
Figure 7 below shows the top 10 occupations that had the highest number of injuries and illnesses in
2019. From an underwriting and counter fraud standpoint, these occupations could serve as a basis for
red flag development and/or higher risk assessment.
Source: Insurance Information Institute. (2021). Facts + Statistics: Workplace Safety/Workers Comp.
https://www.iii.org/fact-statistic/facts-statistics-workplace-safety-workers-comp
b) Existing data pertaining to workers’ compensation fraud cost.
The WCCTF conducted a thorough review searching for existing research available on
workers’ compensation fraud costs. The WCCTF uncovered an extremely credible
research study being performed by the Coalition Against Insurance Fraud’s Workers’
Compensation Fraud Committee. *The WCCTF spoke directly to the committee and
the researchers of the study and reviewed all aspects of the project, including the
methodology and metrics, and deemed that this study was credible and accurately
represented the current state of workers’ compensation fraud. Accordingly, the
WCCTF determined that this 2022 Coalition study will serve as the main resource of
workers’ compensation fraud costs for purposes of this current 2022 study.
*The workers’ compensation statistic that the Coalition Against Insurance Fraud
publishes was deemed as the most credible source as the Coalition has been
supporting the insurance industry with research, advocacy, and support since its
inception in 1993. The Coalition is one of the most well-respected in the anti-fraud
community and provides robust services to consumers, the media, and insurance
organizations.
18
The following excerpt is from the Coalition's Workers’ Compensation Task force and
its research:
The Coalition's Workers Compensation Fraud Task force continues its work of
calculating a new figure that quantifies the amount of comp fraud taking place in the
U.S. Led by Co-Chairs, Dominic Dugo, and Gene Donnelly, the pair has assembled a
multi-disciplinary collective of experts in the field of WC to tackle the assignment of
updating the decades-old $7B estimate. Excluding self-insureds, the committee has
come up with a preliminary estimate of $34B in WC fraud divided between premium
and claim fraud. The committee examined a number of recent studies and reports to
ascertain the value of premium fraud. They also reached out to a number of experts and
academics to capture the cost of claim fraud. Dr. Michael Skiba, PhD and Department
Chair of Criminal Justice at Colorado State University Global, estimated a 16% fraud
rate in the claim volume based on research with dozens of carriers. Based on the 2020
written premium, and using the 16% number, the estimated amount of fraud in WC
claims is
$9B and $25B of premium fraud
. The Committee wants anyone with relevant
expertise or access to authoritative reports/information on fraud in the WC system to
share any information that may better inform their working estimate of $34B. If you have
questions about the committee's methodology or would like to participate in the effort
to update the WC figure, please contact Dominic Dugo at [email protected]g.
c) Research teams’ calculation on the updated cost of workers’ compensation
fraud.
The 2022 Coalition research project focused on two areas of workers’ compensation
fraud to determine their final figure; premium fraud and claim fraud. In analyzing
workers’ compensation claimant fraud it was determined using a base of 2020 written
premiums and multiplying that metric by a 16% fraud rate. A.M. Best provides a direct
written premium in 2020 of $56,225,576,000, which served as the baseline premium
metric. Prior studies performed by the WCCTF resulted in strong indications that 16%
of all workers’ compensation claims are suspicious, thus the use of the 16% figure in
this cost formula. Once written premiums ($56,225,576,000) were multiplied by the
16%, the final result was $8,996,092,160, appropriately rounded to $9 billion as the
final cost of workers’ compensation claimant fraud in 2020.
Workers’ compensation premium fraud was determined by first developing a cost of
fraud in the state of California and then using census data to predict the cost of fraud
countrywide. The baseline used was a $3 billion estimate that was derived by Frank
Neuhauser of the University of California Berkeley who performed a study on the
Underground Economy and Payroll Fraud. The Coalition’s Workers’ Compensation
Task Force used the $3 billion figure and then assumed California's population is 12%

19
of the total United States population (based on 2019 Census Data), the formula was
developed to determine the final cost. According to the United States Census data, in
2019, the U.S. population was 328 million and California was 39.5 million; thus,
California occupies 12% of the total U.S. population.
$3 billion (fraud in California) x 8.3 (California is 12% of the USA population), translates
into a metric of 100 divided by 12 = 8.3. Thus $3,000,000,000 x 8.3 = $24.9 billion
premium fraud in the United States.
The WCCTF, therefore, concludes that workers’ compensation claimant fraud totaled
$9 billion plus $25 billion in premium fraud, for a grand total of $34 billion in workers’
compensation fraud in the United States.
Premium Fraud
a) Introduction to the problem:
Premium fraud also referred to as premium leakage, is a very significant area of
insurance fraud, but is very difficult to assess due to the difficulties when trying to
determine policy misrepresentation on policies. Premium fraud can occur at almost all
points in the policy process, from signing up for a new auto policy to making policy
changes to an existing policy. Policyholders are motivated to misrepresent policy
information since premiums can cost less or more depending on facts that are
provided in the policy application; thus, enticing policyholders to misrepresent certain
facts on their policies in favor of lower premiums. During the initial policy application
process, an insured has the opportunity to misrepresent almost every item covered,
such as drivers, vehicle use, garaging locations, etc. After the policy is in force, the
policyholder can also engage in activity and fail to disclose it to the insurance company
for fear of raising their premium. Some of these activities would include moving to a
higher premium area, allowing a new driver to operate a vehicle, increasing the mileage
driven of a covered vehicle, etc. In addition to this challenge, insurers themselves are
pressured to write policies due to the highly competitive market in that they operate.
This pressure could result in insurers writing a bad risk, which will bring in premiums at
the onset but will be extremely costly to the insurer in the long term due to the high
propensity for fraud in these higher-risk policies.
There are many indicators and common red flags related to premium fraud; the
following are examples of some of these red-flag indicators:
Residency.
• Policy zip code and policyholder area code are in different areas.

20
• Insured is employed a significant number of miles from the policy address.
• Accident is more than a few miles from the policy address.
• Insured is reluctant to meet appraiser/adjuster/investigator at the policy address
and prefers a work location, coffee shop, and the like. This may indicate that
he/she does not reside there.
• Insured agrees to meet the appraiser/adjuster/investigator at residence address
but needs more than a reasonable amount of time to get to the location. Again,
this may indicate that the policyholder does not reside at the address.
• Insured uses a PO box as his or her primary mailing address.
• Insured cannot produce documents that show his or her name and the policy
address—documents such as utility bills, pay stubs, tax returns, or credit card
bills.
Vehicle mileage driven.
• Insured is reluctant to release mileage information via phone or in person.
• Insured avoids appraiser/sales agent/investigator physically viewing the vehicle.
• CARFAX or other database check reveals a significant number of miles in a
short period of time. This may indicate potential commercial use.
• Accidents occurs with multiple passengers that are not related or acquainted
with the insured. This may indicate that the insured uses the vehicle for
commercial or livery use, and potentially the mileage is misrepresented.
Other miscellaneous premium red flags would be as follows:
• Insured pays cash for the premium.
• If insured pays via check, the checks are starter checks.
• Re-employment, the insured is very vague about his/her job duties.
• Premiums seem very high for the insured’s socioeconomic status.
Red flags indicators that can be communicated to first notice of loss report taker:
• Insured provides a PO box.
21
• Multiple people making the loss report.
• Agent documentation indicates that the insured had a higher-than-normal
number of inquiries to the agent prior to loss.
• Insured is hesitant to release personal information and is generally
uncooperative.
• Insured is overly aggressive for a settlement and could also threaten contacting
supervisors, state consumer bureaus, attorneys, etc.
• Insured seems unusually familiar with insurance terms.
• Multiple recent changes in policy coverage, including the coverage that
specifically affects the claim being reported.
(Skiba, 2017)
b) Existing data pertaining to premium fraud cost.
The WCCTF performed an in-depth search canvassing for current research on
premium fraud. After performing this comprehensive search, it was discovered that
there is little to no research performed in the area of premium fraud. The WCCTF’s
extensive search resulted in one study that was performed in 2017 on premium fraud
that was deemed credible and will serve as the foundation for this LOB in this 2022
study. Premium fraud in auto insurance was the focus of a study performed by Verisk
in 2017, which estimated that $29 billion was lost due to premium fraud. *Their
calculation included unrecognized drivers, underestimated mileage, violations,
garaging, and identity exceptions. Significant growth in the use of technology platforms
to write policies (non-face-to-face) makes it easier for an insured to misrepresent items
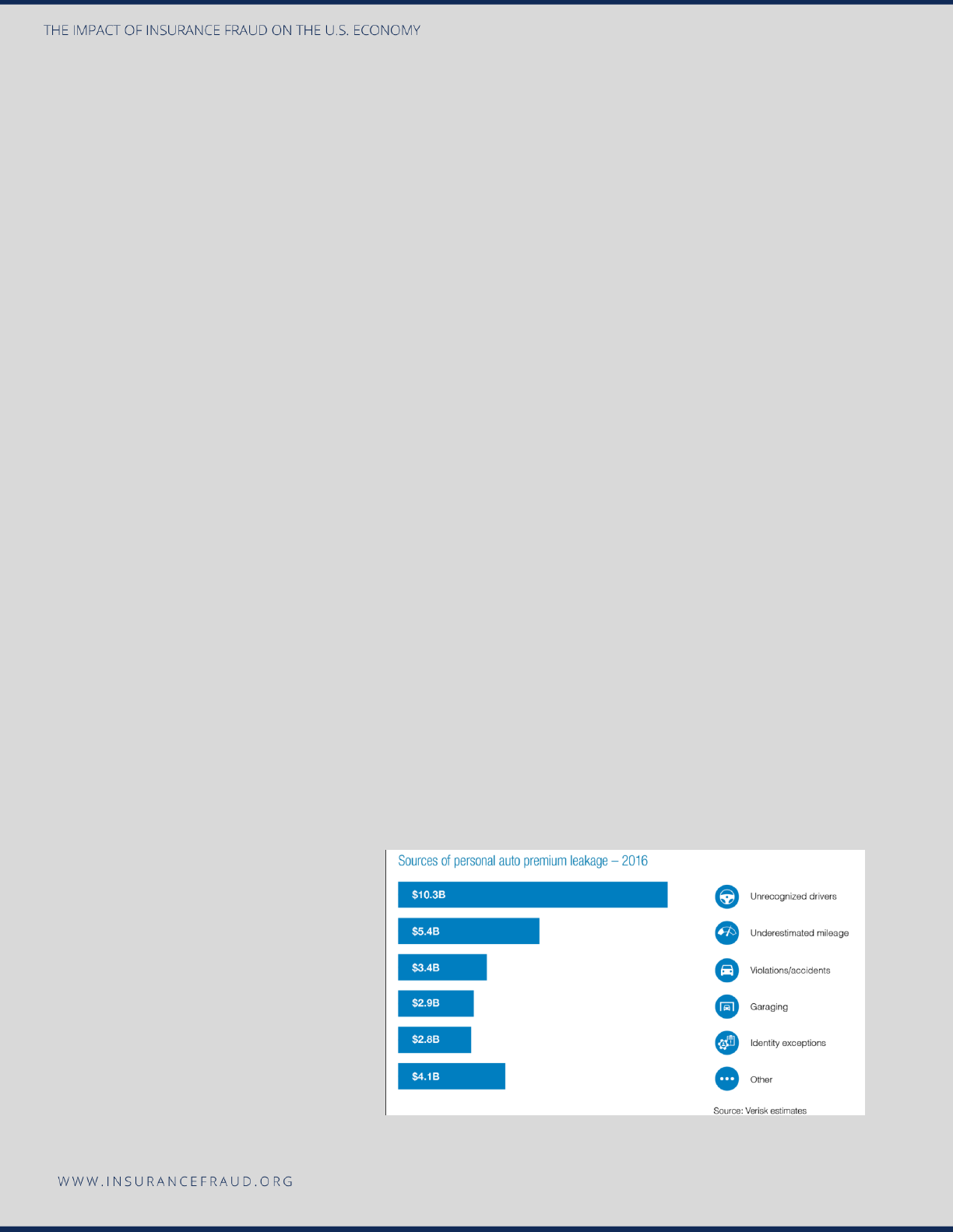
on their policy. As seen below in Figure 8, their study revealed the following sources of
leakage.
Figure 8: Sources of Personal Auto
Premium Leakage
Source: Verisk, 2017.
Due to the lack of other
research uncovered during the
investigation of this LOB, and
the credibility of this study, the
2017 Verisk study will be the

22
primary source of information for this current 2022 study.
*As noted, the Verisk 2017 study was deemed the most effective for the purposes of
this research project. The WCCTF reviewed the Verisk study parameters (copied
below) and accordingly, approved of this methodology as a credible source of data.
“Two Verisk research initiatives support the majority of findings for this Innovation
Paper. The 2016 Verisk Auto Insurance Premium Leakage Survey explored insurers’
concerns, programs, and plans regarding premium leakage. The response represented
58% of private passenger auto insurance premiums. Verisk also conducted a client
analysis for 82 insurers split evenly between standard and nonstandard. The research
combined Verisk’s RISK:check® predictive analytics model that identifies potentially
fraudulent applications with additional data from more than 3 million policies (2.1
million standard, 1 million nonstandard).”
c) Research teams’ calculation on the updated cost of premium fraud.
The 2017 Verisk study will serve as the basis for premium fraud for the purposes of this
study. The Verisk study concluded that in 2017 the cost of premium fraud was $29
billion. If we use a standard Consumer Price Index (CPI) conversion of $29 billion from
2017 to January 2022, we receive a new 2022 cost of fraud of $31.6 billion.
The WCCTF sought a second source to cross-check the final $31.6 billion estimate
derived using the Verisk foundational estimate. To establish a second metric, the
WCCTF used a formula based on the estimated percentage of premium fraud as
established by Reinsurance Group of America (RGA) and then divided that percentage
into the 2020 net written premium for the U.S. A global study performed by RGA in
2017 assessed premium fraud at a rate of 5.9 percent *(Reinsurance Group of America,
2017, Global Claims Fraud Survey). Considering the total net written premium for 2020
($655.5 billion-Figure 9) we derived a formula of $655.5 billion x 5.9 %, which resulted
in a figure of $38.7 billion. When we cross-check this figure of $38.7 billion with the
Verisk figure of $31.6 billion, we can ascertain that both costs are of course different,
but they are within the same range for the WCCTF to be comfortable releasing a new
estimated figure based on these two numbers.
23
Figure 9: Total Net Written Premium 2016-2020 (in billions).
Source: NAIC data, sourced from S & P Global Market Intelligence: Insurance Information Institute.
Regarding the final cost of premium fraud in the U.S., if we take the two figures of
$31.6 and $38.7 billion, and then average these two numbers together, the new figure
for the cost of auto premium fraud in the United States is $35.1 billion.
*The RGA study metric of 5.9% was based on premium fraud in the Americas and did
not isolate The United States from the final 5.9% figure. Despite this shortcoming, the
WCCTF felt that the 5.9% was still the most accurate measure to serve as a baseline
for this project. Regarding the methodology, the RGA conducted an online survey in
September and October 2017 of 27 insurance carriers.
Healthcare Fraud
a) Introduction to the problem:
According to the Centers for Medicare and Medicaid Services (2020, CMS Office of the
Actuary Releases 2019 National Health Expenditures), healthcare spending in 2019
made up nearly 18% of the country’s Gross Domestic Product, totaling $3.8 trillion.
Nearly all of this spending was paid for by insurance. Health insurance has grown in
utilization and popularity across America for the last 100 years when insurance became

24
more widespread following World War I. In 2010, the federal government passed
groundbreaking legislation in the Affordable Care Act. This regulation aimed to give
access to insurance to people that may not have had it prior, and as a result, a large
percentage of Americans are currently covered by health insurance, and most of our
$3.8 trillion annual GDP is paid by health insurance. In a post-Affordable Care Act,
post-Medicaid Expansion America, the United States Census Bureau (2020), estimates
that 92% of people in the U.S. have some form of health insurance. Using those two
figures, an estimated $3.5 trillion in healthcare costs are paid by insurance annually.
Altogether, this makes healthcare a unique and attractive target for fraud, both
because of a large amount of dollars available, and because so much of the spending
is paid by insurance rather than by the individual receiving services.
Insurance fraud schemes can take many forms in healthcare. These schemes are
found in all areas of healthcare, including hospitals, pharmacies, clinics/doctor’s
offices, long-term care facilities, home health services, pharmaceuticals, medical
devices, and durable medical supplies. In some cases, providers bill for services that
were never rendered, which can include billing for services to patients who are
deceased, or who have never seen the provider submitting the claim. Other schemes
involve “upcoding,” or submitting a claim for a service more complex and with a higher
reimbursement rate than the service that was rendered. Upcoding can include billing
for a high quality of medication or supplies, or by inflating complexity. Most provider
visits include an evaluation and management of service. This service can be
reimbursed at multiple rates depending on how complex the patient’s care is and how
difficult evaluating the patient and managing their condition is. Determining the correct
level of complexity is highly subjective, and creates an environment where providers
often determine what level is appropriate on their own. This level of autonomy creates
a large opportunity for fraud.
More complex schemes involve the practice of “unbundling,” where a provider will bill
for each component of a service individually rather than submit a single billing code
that covers all services, as required by some insurance companies. Often a billable
service will include lab work, follow-up, visits, or other auxiliary services that are
supposed to be included in a single rate. Fraud can be committed by submitting claims
for all of the services individually rather than accounting for the included services in the
initial code. Insurances, including both Medicare and Medicaid as well as most
commercial plans, require that a service be medically necessary to be reimbursed. The
provider submitting the claim is often key in determining whether or not the service is
necessary. This allows the provider who will directly benefit from additional services to
manipulate the situation to fraudulently bill by making false statements about a

25
patient’s condition to show medical necessity, including fabricating diagnoses and
misrepresenting the patient’s true conditions.
Healthcare fraud can also be committed by the patient. Medical identity theft has been
becoming more and more common, with uninsured or underinsured persons
presenting to a healthcare provider a name, identification, and insurance information
for a different person. Occasionally, fraud is committed through willing “card sharing”
rather than identity theft. This occurs when a willing person shares their health
insurance information with a family member or friend and helps them impersonate the
insured person when seeking care to get the insurance company to pay for the care
provided to a non-covered person.
b) Existing data pertaining to healthcare fraud cost.
No major commercial health insurance companies report fraud estimates, and national
organizations that do gather this information do not publicly publish it and declined
WCCTF requests for this information. The WCCTF approached approximately 10
carriers and received denials for access to the information they gathered. The WCCTF
located three separate sources of data that were deemed credible for this study. The
National Healthcare Anti-Fraud Association (2019), *is a premier organization in
healthcare fraud and estimates that between 3%-10% of health insurance spending is
lost to fraud nationwide; if we assume the higher 10% metric, fraud costs in health care
could surmount to $300 billion. The WCCTF then used CMS’s 2020 data which shows
$3.8 trillion in total healthcare spending and 2019 United States Census data showing
92% of people in the United States carried health insurance, and calculated as follows:
$3.8 trillion x 92% = $3.5 trillion is paid annually for health insurance claims. CMS data
(as explained in detail in the next lob section on Medicare and Medicaid) shows that
Medicare and Medicaid spending in 2020 totaled $1.5 trillion, meaning the remaining
$2 trillion was paid by commercial insurance plans.
*The NHAFA is seen as the leading healthcare fraud fighting organization in the United
States healthcare industry. They were founded in 1985 and are a private-public
partnership that is comprised of over 100 insurance carriers, law enforcement, and
regulatory agencies. Also affiliated with the NHAFA is the NHCAA Institute for
HealthCare Fraud Prevention, which was established in 2000 and is a separate
educational organization that provides both education and training to anti-fraud health-
care personnel. Accordingly, the WCCTF deems the NHAFA as a highly credible and
reliable source of healthcare research and data.
c) Research teams’ calculation on the updated cost of life insurance fraud.

26
As outlined above, considering the limitations of available statistics (both publicly and
directly from private health carriers) on health care fraud, the WCCTF felt that the most
accurate method to derive at a healthcare fraud metric would be to utilize the data
secured from the NHAFA on fraud percentage (3%) and CMS on total health care
spending ($3.5 trillion). The WCCTF applied the estimated 3% of dollars spent to be
lost to fraud as established by the NHAFA to the $3.5 trillion healthcare expenditures
as established by the CMS. This would suggest total healthcare claims fraud costs all
insurers, including Medicare and Medicaid, $3.5 trillion x 3%= $105 billion annually.
To arrive at an accurate metric on healthcare spending, we must extract from that $105
billion, the amount of fraud in relation to Medicare and Medicaid fraud. Referring to the
next line of business section on Medicare and Medicaid, we derived at a final figure
(averaging AARP and USGOA data) of $68.7 billion dollars to Medicare and Medicaid
fraud. Subtracting Medicare and Medicaid fraud from the total figure leads us to
conclude that fraud costs $36.3 billion per year ($105 billion - $68.7 billion).
Medicare and Medicaid
a) Introduction to the problem:
Medicare and Medicaid are government programs that pay healthcare expenses for
vulnerable populations. Medicare is a federal program focused on elderly and disabled
persons. This is a population that would have less access to traditional health
insurance because private health insurance is often provided through an employer, and
individuals in these populations tend to either be retired or unable to work because of
their disability. Medicare recipients pay an insurance premium and often have other
out-of-pocket costs such as deductibles and coinsurance. The premium is subsidized
by government funds and the provider network and pricing agreements are managed
by the government.
Medicaid is a state-run program that provides access to families living near the poverty
level. Medicaid recipients generally do not pay a premium or out-of-pocket costs. All
costs are paid by the government, which also manages the provider network.
Medicare and Medicaid fraud has a lot in common with traditional healthcare insurance
fraud. Fraud schemes can include billing for services not rendered, upcoding,
unbundling, and providing unnecessary services. Differences are reflected in the nature
of the services provided and the nature of the recipients. Medicare and Medicaid
recipients are more vulnerable to fraud than the general population. Elderly and

27
disabled persons are at higher risk of being fraud victims because they are generally
less involved in the decisions behind their care and may not be as likely to pay close
attention to their bills or may struggle to understand their bills. Since Medicaid
recipients often do not have any cost-sharing, they are less likely to pay attention to
any aspect of billing, making them a larger target. The Department of Health and
Human Services Office of Inspector General considers some services providers to be
at higher risk for committing fraud. Hospitals and physicians are generally considered
lower risk, with Home Health Agencies and Durable Medical Equipment providers
being considered high risk. Because they are more likely to be dealing with life limiting
diseases and decreased functionality, Medicare and Medicaid patients are more likely
to receive services from high-risk providers than the population covered by traditional
insurance. The government also spreads more resources on investigating and
pursuing fraud over private, commercial, insurance companies. This suggests that
Medicare and Medicaid would experience more fraud than commercial insurance
companies.
b) Existing data pertaining to Medicare & Medicaid fraud cost.
The WCCTF conducted an exhaustive search canvassing for metrics on Medicare and
Medicaid fraud and found an incredibly wide range and inconsistent results, such as
metrics of $60 billion annually from the University of Southern California Center for
Elder Justice (2021) to $134 billion from the Center for Medicare and Medicaid
Services (2020) and even groups such as the Center for to the National Conference of
State Legislatures (2022) concluded that fraud in Medicare and Medicaid is nearly
impossible to measure. The CMS was seen as a very credible source by the WCCTF,
but after deep analysis into the $134 billion figure they derived at, it was decided to
refrain from including the metric in the final analysis. CMS themselves estimated $134
billion (2020), annually in improper Medicare and Medicaid claims, however, they point
out that not all improper claims were necessarily fraud. The WCCTF arrived at the $134
billion figure by adding up the 2020 Improper Payments from FFS, Part C, Part D,
Medicaid, and CHIP dollars from the chart in the citation above from the CMS website.
This $134 billion number includes waste and abuse, which may be unintentional, such
as a misunderstanding or a disagreement about when there is an honest, good-faith
question regarding medically necessary. This figure also follows Office of Management
and Budget Office guidance that any claim unsupported by documentation is assumed
to be improper rather than undetermined. It was therefore decided to refrain from
including the CMS number of $134 billion as part of this study.
The WCCTF scoured for other sources and located two other highly credible sources
that will be utilized for this line of business. The American Association of Retired

28
Persons (AARP), referencing United States General Attorney Jeff Sessions, estimates
that CMS pays $1,000 in fraud claims per member, or roughly $60 billion (2018). *
The United States Government Accountability Office (USGOA) puts the number a little
higher, at $77.4 billion (2019). *The WCCTF derived at $77.4 billion by referring to the
report, which states $36.2 billion for Medicare Fee-for-service/FFE and another $41.2
billion for Medicaid, which summed together, total $77.4 billion.
*AARP is the nation’s largest non-profit organization representing individuals over 50.
Having roughly 40 million members in the United States, it is considered the most
credible and robust organization focusing on matters of that age group. Accordingly,
this organization is known to provide highly detailed and accurate research and
reporting on topics related to individuals over 50, such as Medicare and Medicaid.
*The United States Government Accountability Office is a legislative branch
government agency that provides auditing, evaluation, and investigative services for
the United States Congress. Their primary function is to investigate and monitor federal
spending and performance. As they are the top agency in the United States that
monitors federal spending, they are an ideal resource to provide data and research for
this study.
c) Research teams’ calculation on the updated cost of life insurance fraud.
The WCCTF calculated a final number for Medicare and Medicaid fraud by taking an
average of the AARP ($60 billion), and the USGOA ($77.4 billion) figure, $60 billion +
$77.4 billion = $137.4 billion divided by 2 = $68.7 billion. Although some sources do
not consider Medicaid to be insurance as there is technically no risk sharing, the
general population considers it to be a form of insurance, and it functions from a billing
perspective similarly to Medicare and other commercial insurers. Therefore, the
WCCTF believes Medicare and Medicaid fraud should both be included in the total
amount.
Life Insurance Fraud
a) Introduction to the Problem:
Life insurance fraud is deliberate deception committed by an insured or insurance
agent to gain a financial advantage. Applicants, policyholders, third-party claimants,
and professionals who provide services are all potential fraud sources. Misrepresenting
life insurance policy information, tampering with another person’s policy, and fake
deaths, are among the common frauds. Life Insurance fraud is one of the most serious

29
problems facing insurers, insurance consumers, and regulators. Its existence not only
increases the cost of insurance but also threatens the financial strength of insurers and
negatively affects the availability of insurance. Insurance fraud encompasses a wide
range of illicit practices and illegal acts involving intentional deception or
misrepresentation. Some of the most common forms of life insurance fraud include:
● Lying on an application. This involves adjusting, or even withholding valuable
information, such as any medical conditions.
● Forgery. A common scheme is when someone other than the policyholder will
change a beneficiary.
● Fake policy. Fake agents sell fake policies that do not exist and pocket the
money.
● Faked death. In these instances, people try to collect for someone who is still
alive or never existed.
● Murder. When a beneficiary plans to kill a policyholder and pocket the payout.
● Pocketing premium. An agent pockets the premium payment instead of
forwarding it to the company.
Life insurance policies also involve a contestability period, that is, the time frame in
which an insurer can deny a claim for material misrepresentation and fraud. This period
varies by state, but it is generally one to two years. Research by the Reinsurance
Group of America (2017) reveals that 20% of life insurance policies are rescinded by
insurance companies.
b) Existing data pertaining to life insurance fraud cost.
The WCCTF performed a robust search looking for current data on life insurance fraud
and unfortunately, very limited information was revealed. The WCCTF searched every
potential platform in search of research on life insurance fraud statistics including open
source, direct industry contacts with the III, NAIC, FBI, the Coalition, ACFE, IASIU, and
academic libraries. As a result of that exhaustive search only one study that was
conducted in 2017 by the Reinsurance Group of America (RGA) was found. All other
sources that were located that focused on life insurance fraud made reference to the
2017 RGA study, confirming that the RGA study was the only research study
completed focused on life insurance fraud.
To understand the life insurance fraud problem the RGA surveyed 25 insurance
carriers, conducted informational interviews among insurance carriers, held information
gathering discussions at the 2016 RGA Annual Fraud Conference, and conducted their
internal research of the claims experience. Based on that method, the RGA reported
that they estimate life insurance fraud to cost approximately $10-20 billion each year.
30
The RGA further states that 1%-3% of all life insurance claims are either investigated
for fraud or misrepresentation, or they are denied outright.
c) Research teams’ calculation on the updated cost of life insurance fraud.
In considering the research revealed in section b above, it was determined that a new
figure for the cost of life insurance fraud would be necessary. Although the 2017 RGA
study added insights and was the most cited in terms of life fraud, the methodology
was based on several survey instruments, and even though this could be a very
credible source of information, without knowing the details of the survey instruments,
the research protocols, the sample, etc., the WCCTF felt that a new cost was needed.
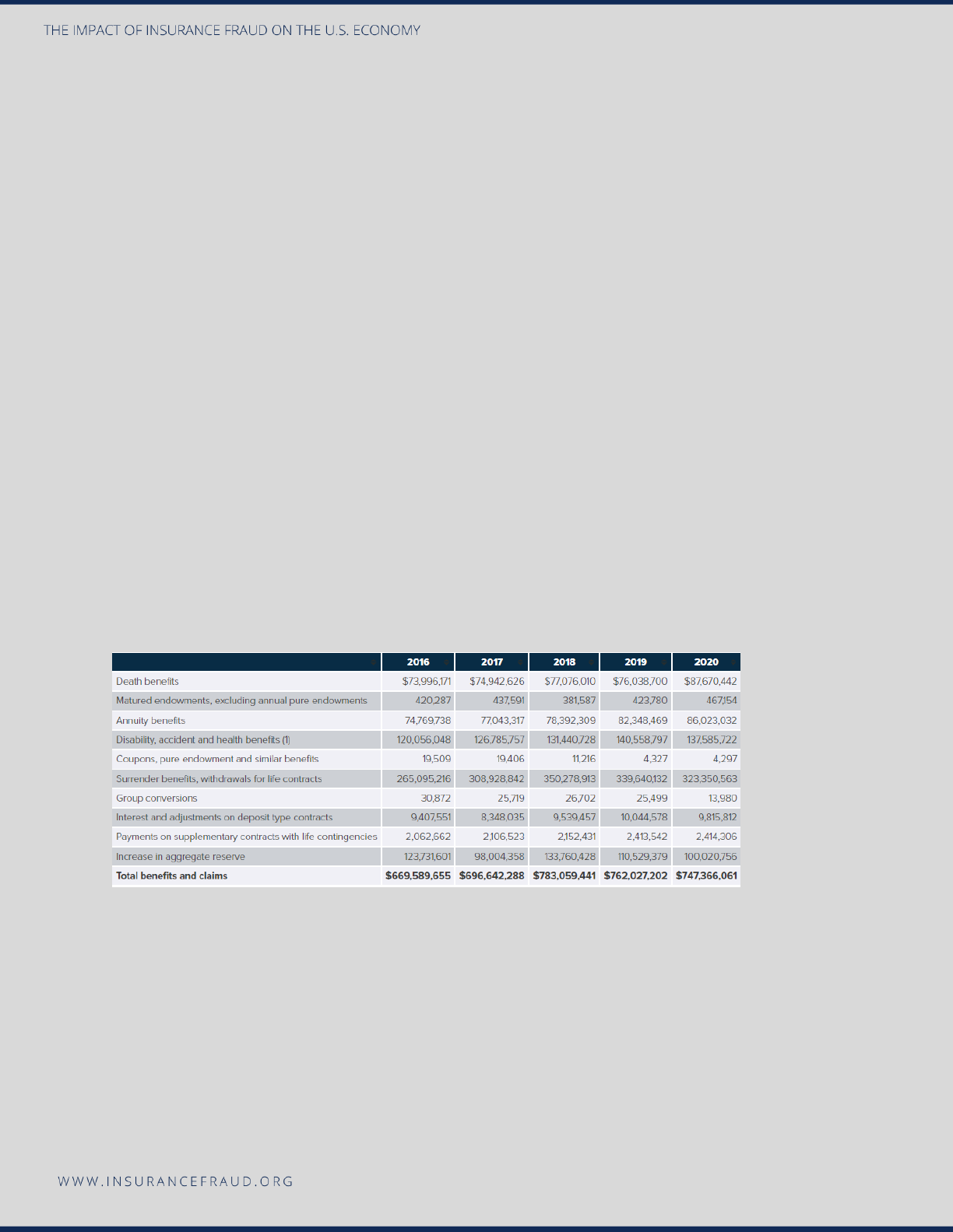
To arrive at a new formula for life insurance fraud, the WCCTF looked for data on the
total life insurance benefits and claims paid in past years. A very credible and accurate
source was uncovered when the WCCTF located data published by the III. *(Insurance
Information Institute, 2021, Insurance Fact Book Payouts). As seen by Figure 10 below,
a recent study by the Insurance Information Institute (III) showed life insurance benefits
and claims reached $747.4 billion in 2020. The amount includes death benefits from life
insurance, annuity payments, disability payments, and other payouts. It is interesting to
note when analyzing data in this form that life insurance benefits have slowly declined
since 2018.
Figure 10: Life Insurance Benefits and Claims 2016-2020
Source: Insurance Information Institute, 2021, Insurance Fact Book Payouts.
Key fraud organizations such as NICB, III, the Coalition, NAIC, and IASIU, widely
circulated the figure of 10% as the key percentage of claims that are fraudulent.
Accordingly, the WCCTF will propose a new cost of life insurance fraud using the total
benefits and claims payout as indicated by the III in Figure 10 above and then use the
metric that 10% of all life claims are fraudulent as a baseline. Using this formula, if the
life insurance benefits and claims payout was $747.4 billion in 2020, and we estimate
that approximately 10% of that figure was fraudulent we would derive at a new cost of

31
$747.4 billion x 10% = $74.7 billion. Therefore, the 2020 estimate of life insurance fraud
in the United States is $74.7 billion.
The increasing number of life insurance frauds not only increases costs for the
companies but also leads to inflated premiums, which is felt by consumers. Therefore,
it is necessary to have a proper risk management framework to curtail or minimize life
insurance fraud. A life insurance company’s commitment to fraud control will be met
by identifying the opportunities for fraud and implementing risk avoidance, its
prevention, and procedures for its minimization in the day-to-day system of operations.
*As already noted in the property and casualty line of business section earlier, the
Insurance Information Institute was chosen as the most reliable, credible, and effective
data source as the III is one of the most well-respected members of the insurance
industry. Since 1960, the III has been one of the most trusted sources of data for
consumers, the media, and professionals in the insurance industry and at its core
organizational function researches and publishes information, statistics, and data on
the insurance industry.
Disability Insurance Fraud
a) Introduction to the Problem:
Disability fraud involves making a false statement, providing incorrect information, or
withholding information to collect benefits (individual or group). There are many forms
of disability fraud, including; faking a medical issue to be declared disabled, continuing
to collect payments after the individual has recovered, receiving benefits while working
another job, usually “off the books”, exaggerating a medical condition to meet the
disability threshold for collection and inflating income on a Social Security Benefits
application to increase payout.
In reviewing the current literature related to disability fraud, there appear to be many
inconsistencies in its definition and measurement. Some sources include disability in
workers’ compensation fraud, some consider it an entirely separate line of business,
and yet others define it separately, but segment it as being fraud against private
carriers and the Social Security Administration. It is also readily labelled “improper
payments” by the Social Security Administration. Due to these inconsistencies and the
wide variety of definitions, parameters, costs, and statistics being circulated, the
WCCTF decided to focus on Social Security Disability fraud as the primary area of
study as these statistics are well defined in the literature.
32
b) Existing data pertaining to premium fraud cost.
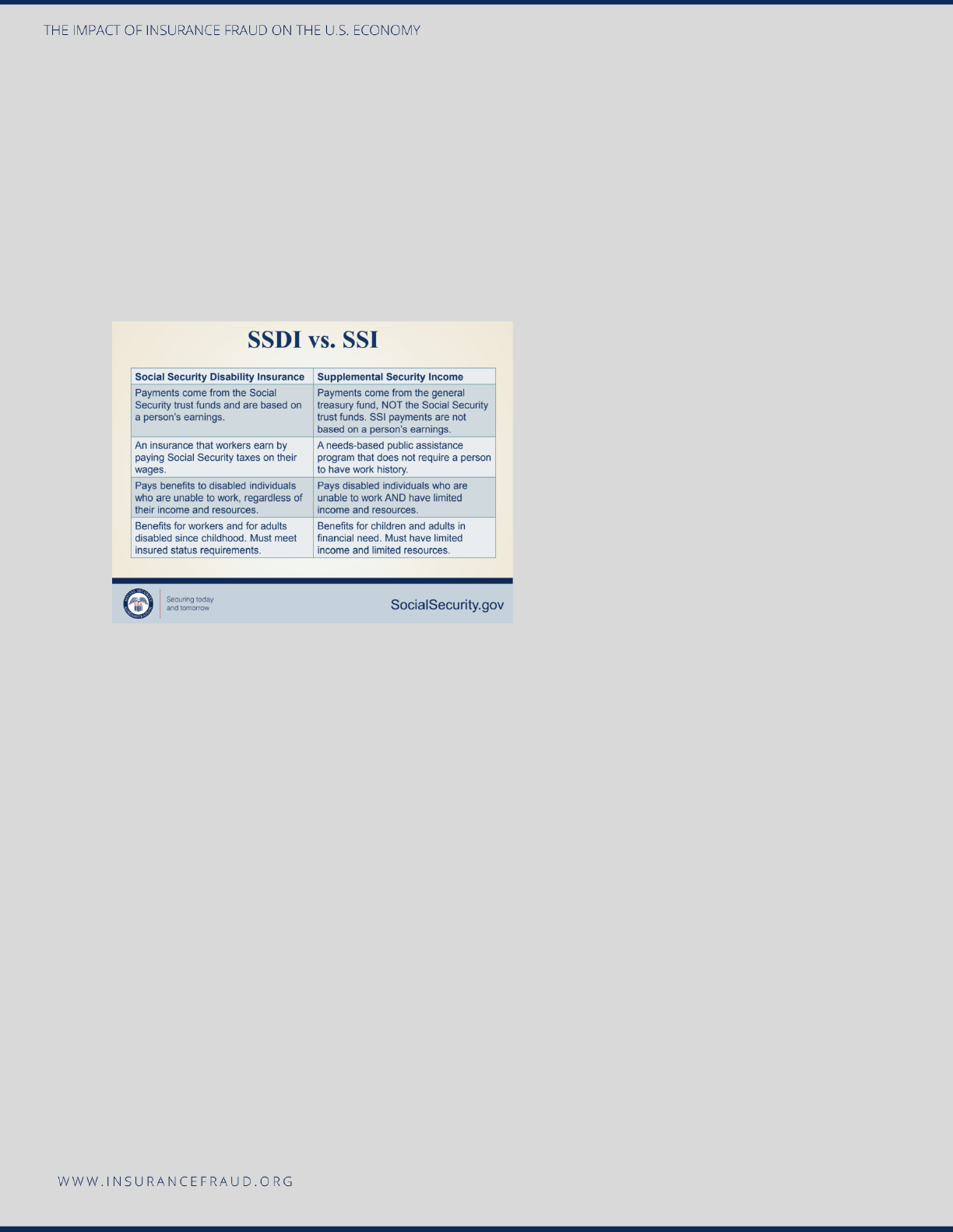
The Social Security Disability Insurance (SSDI) and Supplemental Security Income (SSI)
programs offer assistance to individuals that are disabled. SSDI pays a benefit to an
injured party or family member if you are an eligible worker and have paid Social
Security taxes on your income. SSDI will reimburse individuals with disabilities who
have limited income. The table below (Figure 11) shows the highlights of the difference
between SSDI and SSI (Social Security Administration, 2022).
Figure 11: Comparison of SSDI vs. SSI
Source: Social Security Administration, 2022.
As previously mentioned, the WCCTF
will focus on Social Security
Disability fraud, or Improper
Payments, as the focal point for
developing a cost current 2022 cost
of disability fraud. The WCCTF
performed an exhaustive search for
credible and accurate data pertaining
to disability insurance and located
several interesting sources but decided for the purposes of this study to utilize data
from the most seminal organization in this area, the Social Security Administration
(SSA). As the SSA is the top branch of the United States government that oversees life
insurance and therefore the data and research they publish is an ideal fit for purposes
of this study.
The Social Security Administration (SSA) considers payments to be improper, “…if they
result from a mistake in computing the payment, its failure to obtain or act on available
information, a beneficiary’s failure to report an event, or a beneficiary’s incorrect
report”. The SSA considers improper payments to comprise of both under and
overpayments; underpayments when they mis-calculate benefits, and overpayments
when they pay someone more than they are due. The SSA estimated that in 2019, a
total of $7.9 billion was paid in total improper payments (Social Security Administration,
2020).
c) Research teams’ calculation on the updated cost of life insurance fraud.
As the SSA data is incredibly reliable, robust, and accurate, the WCCTF focused on
data published by the SSA as the basis to develop the new cost of disability fraud in

33
the United States. The SSA estimated that in 2019, $7.9 billion was paid in improper
payments, that is, both overpayments and underpayments (defined in section b above).
As underpayments are payments that the SSA makes as a result of improper
calculation, and potentially an error on behalf of the SSA, it was decided that because
these types of payments are not necessarily fraudulent, the WCCTF will refrain from
including underpayments in the final cost of disability fraud. In other words, the
WCCTF will only focus on overpayments as these payments can be precipitated by
insured and beneficiary misrepresentation and fraud. We conclude that our new cost of
disability insurance fraud will be based on SSA overpayments. As published by the
SSA in their Fiscal Year 2020 Agency Report, they estimate that it made $6.6 billion in
overpayments in 2019 (Social Security Administration, 2020).
Accordingly, if we use a standard Consumer Price Index (CPI) conversion of $6.6 billion
in 2019 to January 2022, we receive an 81.5% inflation rate, which would convert into
a 2022 cost of disability fraud in the United States as $7.4 billion!
Auto Theft*
a) Introduction to the problem:
The FBI’s Uniform Crime Report (UCR) defines motor vehicle theft as the theft or
attempted theft of a motor vehicle. A motor vehicle is formally defined as a self-
propelled vehicle that runs on land surfaces and not on rails and could include sport
utility vehicles, automobiles, trucks, buses, motorcycles, motor scooters, all-terrain
vehicles (ATV), and snowmobiles. The following are not considered motor vehicles
according to the UCR; farm equipment, construction vehicles (bulldozers, etc.),
airplanes, and boats (Federal Bureau of Investigation, 2020). It is interesting to note that
the UCR considers the taking of a motor vehicle for temporary use by persons having
lawful access as being excluded from this definition of auto theft.
Auto theft is always evolving, thus creating a very challenging atmosphere for
companies and agencies that are tasked with investigating these crimes. Auto thieves
are very savvy at pivoting to new and sophisticated methods for theft, including smart
keys, cloning vehicles, and using false identities to purchase high-end luxury vehicles.
b) Existing data pertaining to premium fraud cost.
The research team explored all possible sources for accurate statistics and metrics on
auto theft and as a result, several key sources were identified. The National Insurance
Crime Bureau (NICB) maintains an accurate database on auto theft as it affects the
general consumer population and specific industry members of NICB. Additional theft
data was also discovered that is maintained by the Insurance Information Institute (III).
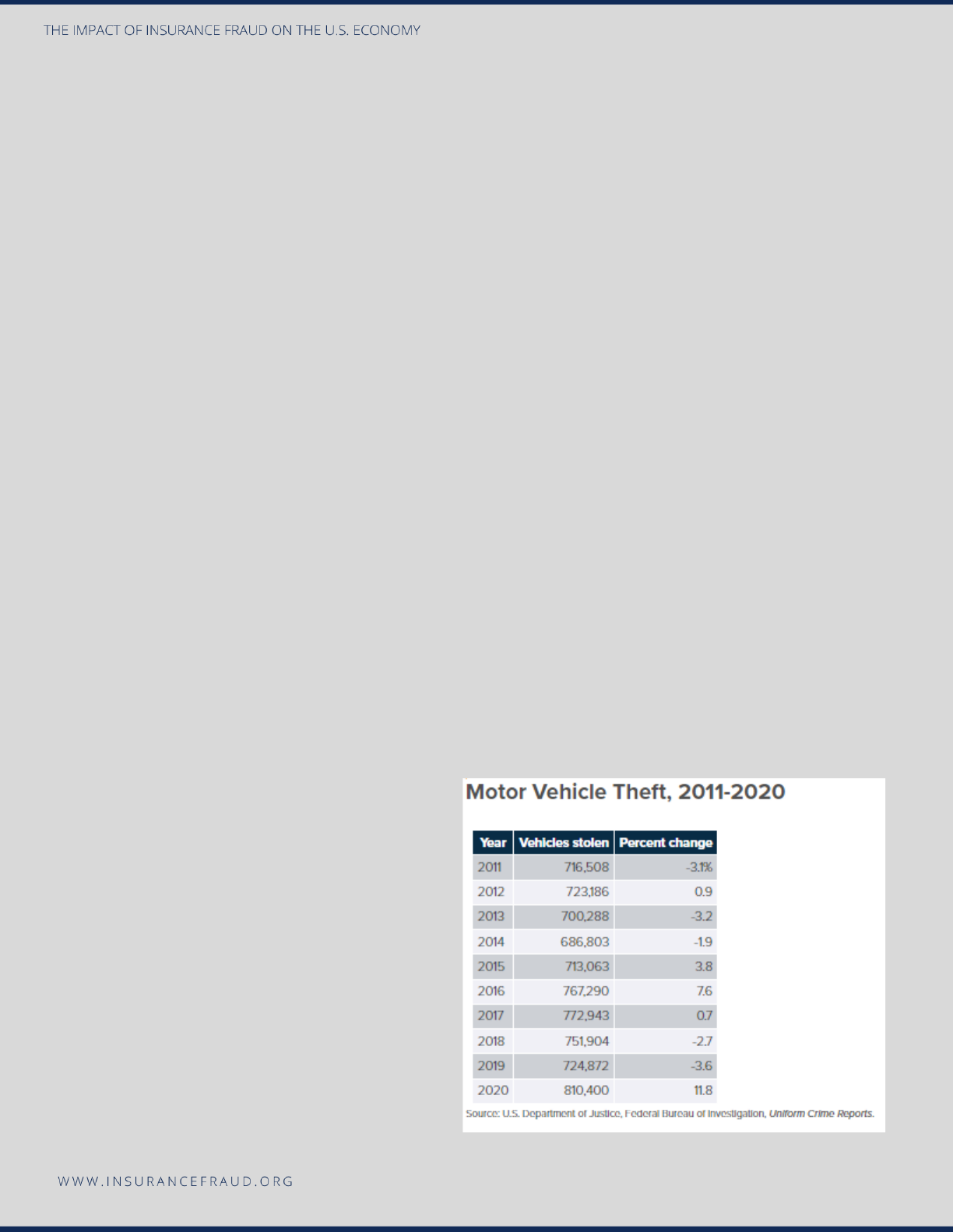
34
The NICB and III data are very accurate and meaningful and were considered as part of
this analysis, however, the data gathered and maintained by the FBI was used as the
primary source for this current research study for the following reasons. The FBI
defines auto theft as a key component in their robust UCR measurement and has been
maintaining auto theft records for many decades; thus, the FBI was considered one of
the primary sources of auto theft data for this study. In reviewing the 2019 and 2020
UCR in detail, some key highlights are:
2019
• Total thefts nationwide: 724,872.
• The rate of motor vehicle theft was 219.9 per 100,000 inhabitants.
• Of all the classifications of motor vehicles as defined by the UCR (in the above
paragraph), automobiles ranked the highest at 74.5% of the total.
• The average value of auto theft was $8,886.
2020
• The average dollar loss per theft was $9,166.
• 810,400 vehicles were stolen, the highest yearly number of vehicles stolen since
2008 (959,059). See Figure 12.
• The number of thefts increased 11.8 % from 724,872 in 2019.
• The rate of motor vehicle theft was 246 per 100,000 inhabitants, the highest rate
since 2009 (259).
(Federal Bureau of Investigation, 2020)
Figure 12: Motor Vehicle Theft Rates 2011-2020
Source: U.S. Department of Justice, Federal Bureau
of Investigation, Uniform Crime Reports.
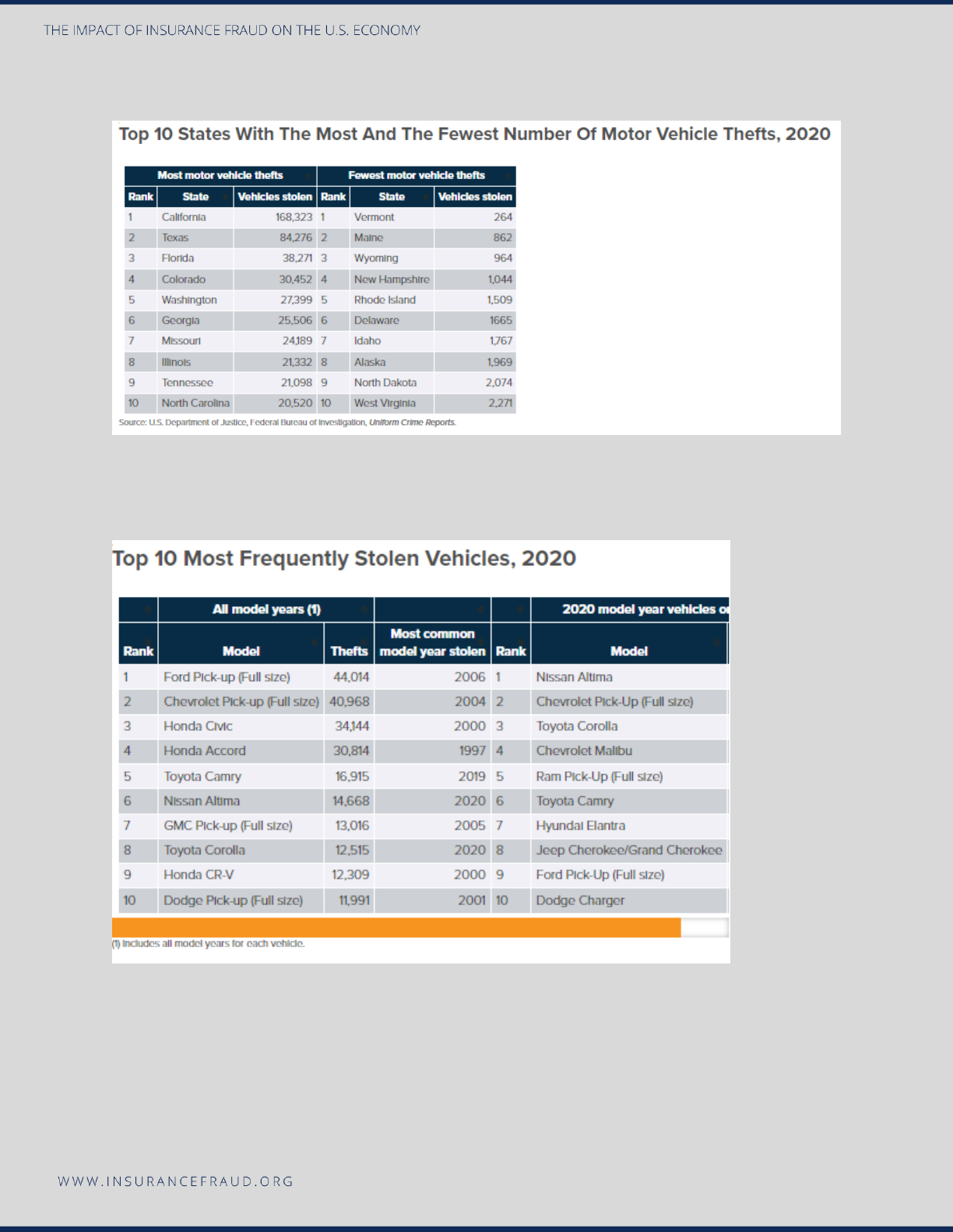
35
Figure 13: Motor Vehicle Theft-States with the Highest and Fewest
Source: U.S. Department of Justice, Federal Bureau of Investigation, Uniform Crime Reports.
Figure 14: 2020 Top 10 Most Stolen Vehicles
Source: NICB, 2020, NICB Releases Annual “Hot Wheels” report: America’s Top Ten Most Stolen Vehicles.
https://www.nicb.org/news/news-releases/nicb-releases-annual-hot-wheels-report-americas-top-ten-
most-stolen-vehicles

36
Auto theft was on the rise in 2020, with a total of 810,400 thefts occurring. NICB
estimates in 2020 that 1 car was stolen every 36 seconds (NICB calculated this
statistic based on 880,595 thefts occurring). Auto theft over the past five years (2016-
2020) remained around 800,000, but the five-year peak in 2020 was attributed to
several factors, most notably, the pandemic, economic downturn, owner complacency,
loss of juvenile outreach programs, and public safety budgetary and resource
limitations. When we analyze geographic regions, the west coast (California, Oregon,
Nevada, and Washington) and mid and southwest (Colorado, New Mexico, Missouri,
and Kansas) had the highest rates of car theft in 2020 (Federal Bureau of Investigation,
2020; Insurance Information Institute, 2021).
Considering the information presented above regarding the measurement of auto theft,
the WCCTF fully discloses that the final formula that was used for purposes of this
study to derive a new cost of auto theft is not the most ideal to accurately measure this
line of business. Of all of the lines of business studied in this research project, this line
of business is seen as the one that has the most significant limitations regarding
gathering. Specifically, the WCCTF would like to note that the FBI statistic, although
they clearly define their data as “auto theft”, measures auto theft as a whole and does
not necessarily differentiate between auto theft as a crime and auto theft resulting from
insurance fraud Therefore, it is noted that this measurement does have limitations,
however, the WCCTF felt that even with these limitations, the final figure that was
derived at should be included in this study.
c) Research teams’ calculation on the updated cost of auto theft.
The WCCTF considered all of the data that was uncovered by researching the NICB, III
and FBI statistics, but the metric as circulated by the FBI will be used as the primary
source of auto theft cost for this 2022 study. As stated, and defined earlier in this
section, the FBI maintains very accurate and robust data pertaining to auto theft
statistics in the United States. Therefore, the cost as calculated and communicated by
the FBI will be utilized for this study. Accordingly, the FBI estimates that the total cost
of motor vehicle theft in the United States for 2020 is $7.4 billion (Federal Bureau of
Investigation, 2020; Insurance Information Institute, 2021). Therefore, $7.4 billion will be
the current cost estimate of auto theft for purposes of this study.
VI. Compilation of LOBs into a final 2022 estimate of
insurance fraud cost
This section will consist of compiling all of the LOBs into one final estimate of the cost
of insurance fraud in the United States as of 2022.
37
● Property and Casualty Fraud. The WCCTF estimates that the current cost of
Property and Casualty fraud in the United States is $45 Billion.
● Workers’ Compensation Fraud. The WCCTF estimates that workers’
compensation fraud totals $34 billion in the United States.
● Premium Avoidance or Misclassification. The WCCTF estimates premium fraud
in the United States is $35.1 billion.
● Healthcare Fraud. The WCCTF estimates healthcare fraud in the United States is
$36.3 billion.
● Medicaid and Medicare Fraud. The WCCTF estimates Medicaid and Medicare
fraud in the United States is $68.7 billion.
● Life Insurance Fraud. The WCCTF estimates that life insurance fraud in the
United States is currently $74.7 billion.
● Disability Fraud. The WCCTF estimates that the current cost of disability fraud in
the United States is $7.4 billion.
● Auto Theft. The WCCTF estimates auto theft in the United States is $7.4 billion. *
FINAL ESTIMATE OF THE COST OF INSURANCE FRAUD IN THE
UNITED STATES:
(All numbers are in billions and figures are as of 2022)
Property & Casualty $45B
Workers’ Compensation $34B
Premium Avoidance $35.1B
Healthcare $36.3B
Medicare and Medicaid Fraud $68.7B
Life $74.7B
Disability $7.4B
Auto
Theft* $7.4B
$308.6 Billion Annually
VII. Statement on Auto Theft
This report includes auto theft in the analysis of the updated estimate of the cost of
insurance fraud in the United States. At the current time, auto thefts in the United
States are reported to be on the rise. These thefts directly impact insurers through

38
increased claims, investigations of the theft, and policy payments where appropriate.
Auto thefts also harm consumers. Obviously, those directly impacted are harmed but
so too are all consumers who pay for auto theft crimes through higher premiums.
Absent provable involvement of the insured in the theft, however, auto theft is not
insurance fraud but an insurance crime for which virtually all automobile insurance
policies extend coverage. The Coalition recognizes the extensive and excellent work
being done by our partner, the National Insurance Crime Bureau, law enforcement
agencies and others to fight back on the crime of automobile thefts. We include the
information in this report, and the cost in our estimate of insurance fraud cost in the
United States to assist those efforts and shed additional light on the problem of
automobile thefts in our nation.
VIII. Recommendations for future study
The WCCTF is honored to embark on such an incredibly insightful journey exploring
the world of insurance fraud and investigating the many different aspects of this unique
form of white-collar crime. Throughout the study, the WCCTF saw opportunities for
further research and investigation for others seeking to dive deeper into estimating the
cost of insurance fraud. Specifically, the WCCTF would recommend researching each
of these LOB’s through an entirely separate study, or studies, to take a deep dive into
the intricate areas of each LOB. Focusing initially on one specific LOB would prove
fruitful as this would allow the team to myopically explore a survey instrument, develop
committees, and create a highly focused methodology. Additionally, the WCCTF
recommends a research group be created dedicated to gathering and compiling fraud
measurements across all LOB’s on a regular and ongoing basis. Having a consistent
picture of the cost of insurance fraud would assist with the allocation of current and
hopefully increased resources in this endeavor.
IX. Conclusion
This report has quite literally been a quarter-century in the making. It is doubtful
anyone associated with creation of the original $80 billion estimate of the cost of
insurance fraud would have foreseen their work creating the most cited anti-fraud
statistic in the United States. Federal and state agencies, courts – both federal and
state, regulators, legislators, insurers, national and international media and academic
research all routinely cite to that original figure.
In 2021 the Coalition Against Insurance Fraud embarked on this project to provide
each of these important stakeholders, and more importantly America’s consumers,
with a far more accurate and up-to-date estimate of the cost of insurance fraud on our

39
nation’s economy. This report is the result of that endeavor. We again wish to express
our great appreciation to those who partnered with us on this task: the National
Insurance Crime Bureau, the International Association of Special Investigation Units,
the American Property & Casualty Insurance Association, and the Insurance
Information Institute. Our greatest appreciation, however, goes to the incredible team
at the Colorado State University Global White Collar Crime Task Force, led by Dr. J.
Michael Skiba. Their dedication, spirit and untold hours of work form the foundation
upon which this vital report is based.
X. Appendix
Recommendation for the measurement of fraud
Many inquiries were received from the Coalition members requesting a
recommendation as to how to accurately measure fraud. As a result of this demand,
the WCCTF directs those seeking more information to an excerpt from Dr. J. Michael
Skiba’s book entitled “The Psychology of Fraud”.
In that book, an entire chapter is devoted to addressing this exact topic. The WCCTF
hopes that this appendix section will serve as a guide for insurance companies to
assist with the development of an effective measurement formula to integrate into their
respective organizations. The data that insurance companies gather and maintain
concerning fraud is incredibly valuable as it provides incredible insights as to the
nature of fraud occurring within their respective organizations. However, this data is
also extremely useful to consumers as it is the backbone of showcasing the damaging
effect of fraud. In addition, legislators and the legal environment can also benefit from
this data as they can also use it to make highly strategic and effective decisions about
fraud and prevention.
To review the Appendix in full please visit this site:
https://insurancefraud.org/wp-content/uploads/Appendix-THE-IMPACT-OF-
INSURANCE-FRAUD-ON-THE-U.S.-ECONOMY.pdf
40
XI. References
Actuarial Standards Board (2022). Loss Adjustment Expense. http://www.actuarialstandardsboard.org/?s=loss+adjustment+expense+&submit=
Aleksandrowicz, P. (2020). Verification of Motor Vehicle Post Accident Insurance Claims. Transport Problems, 15(1), 25. https://doi.org/10.21307/tp-2020-003
Altermark, N., & Nilsson, H. (2020). State Measurements of Benefit Fraud: Why Expert Elicitations Cannot Be Used to Measure Incorrect Personal Assistance Payments. Scandinavian Journal
of Disability Research, 22(1), 158. https://doi.org/10.16993/sjdr.610
American Association of Retired Persons. (2018). April AARP Bulletin Special Report. https://press.aarp.org/2018-4-2-April-AARP-Bulletin-Special-Report
Baranek, D., & Sanchez, M. H. (2018). The Tricare Fraud: A Case Study in Data Analytics for Healthcare Fraud Detection. Journal of Accounting & Finance (2158-3625), 18(8), 10–17.
https://doi.org/10.33423/jaf.v18i8.107
Bureau of Labor Statistics. (2022). News Release-Employer Cost for Employee Compensation. ecec.pdf
Business Insurance (2018). Claim denials, Not Report Lag, Lead to Rising Comp Costs. https://www.businessinsurance.com/article/20180613/NEWS08/912321979/Claim-denials-not-report-
lag-lead-to-rising-workers-compensation-costs
Callaway, J., et al. (2016). Investigating Life Insurance Fraud and Abuse: Uncovering the Challenges Facing Insurers. Retrieved from https://www.rgare.com/docs/default-source/newsletters-
articles/fraud-white-paper.pdf?sfvrsn=a7ffa6880
Centers for Medicare & Medicaid Services. (2020). 2020 Estimated Improper Payment Rates for Centers for Medicare & Medicaid Services (CMS) Programs.
https://www.cms.gov/newsroom/fact-sheets/2020-estimated-improper-payment-rates-centers-medicare-medicaid-services-cms-programs
Centers for Medicare & Medicaid Services. (2020). CMS Office of the Actuary Releases 2019 National Health Expenditures. https://www.cms.gov/newsroom/press-releases/cms-office-
actuary-releases-2019-national-health-expenditures#:~:text=The%20growth%20in%20total%20national,trillion%2C%20or%20%2411%2C129%20per%20person.
Centers for Medicare & Medicaid Services. (2021). Historical. Retrieved from https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-
Reports/NationalHealthExpendData/NationalHealthAccountsHistorical
Chandler, S. J. (2020). Medicare for All: The Need for a Long Approach. Houston Journal of Health Law & Policy, 20(1), 1–65.
Coalition Against Insurance Fraud. (2022). Workers Compensation Study to be released June 2022.
Coalition Against Insurance Fraud. ( 2021). Fraud Stats. Retrieved from https://insurancefraud.org/fraud-stats/
Coustasse, A. (2021). Upcoding Medicare: Is Healthcare Fraud and Abuse Increasing? Perspectives in Health Information Management, 18(4), 1–14.
Federal Bureau of Investigation. (n.d.). Insurance Fraud. Retrieved November 15, 2021, from https://www.fbi.gov/stats-services/publications/insurance-fraud
Federal Bureau of Investigation. (2020). 2019 Crime in the United States. Motor Vehicle Theft. https://ucr.fbi.gov/crime-in-the-u.s/2019/crime-in-the-u.s.-2019/topic-pages/motor-vehicle-theft
FRISS. (2020, November 10). Insurance Fraud Report 2020: The Impacts Of COVID-19 On AI
And Digitalization in Insurance. Retrieved from https://www.friss.com/press/insurance-fraud-report-2020-the-impacts-of-covid-19-on-ai-and-digitalization-in-insurance/
Insurance Council of Texas. (2022). Workers’ Compensation Fraud – It’s Real and It’s A Problem https://www.insurancecouncil.org/workers-compensation-fraud/
Insurance Information Institute. (2021). Insurance Fact Book Payouts. Retrieved from https://www.iii.org/publications/2021-insurance-fact-book/life-annuity-financial-data/payouts
Insurance Information Institute. (2021). Facts + Statistics: Auto theft. https://www.iii.org/fact-statistic/facts-statistics-auto-theft
Insurance Information Institute. (2021). Facts + Statistics: Industry overview. https://www.iii.org/fact-statistic/facts-statistics-industry-overview
Insurance Information Institute. (2021). Facts + Statistics: Workplace Safety/Workers Comp https://www.iii.org/fact-statistic/facts-statistics-workplace-safety-workers-comp
Insurance Research Council (2015). Insurance Research Council Finds That Fraud and Buildup Add Up to $7.7 Billion in Excess Payments for Auto Injury Claims. IRC Fraud News Release.pdf
Islam, M. R., Liu, S., Biddle, R., Razzak, I., Wang, X., Tilocca, P., & Xu, G. (2021). Discovering dynamic adverse behavior of policyholders in the life insurance industry. Technological
Forecasting & Social Change, 163. https://doi.org/10.1016/j.techfore.2020.120486
Kerr, D. A. (2021). A replication study of moral hazard in bodily injury liability auto insurance claims filing decisions. Risk Management & Insurance Review, 24(4), 401.
Kess, S., Grimaldi, J. R., & Revels, J. A. J. (2017, September 1). Covering risks through property/casualty insurance. The CPA Journal, 87(9), 66.
Knopf, A. (2021). OIG finds about $17 million in improper costs in HRSA mental health grants. Brown University Child & Adolescent Psychopharmacology Update, 23(1), 6–8.
Kotekani, S. S., & Velchamy, I. (2020). An Effective Data Sampling Procedure for Imbalanced Data Learning on Health Insurance Fraud Detection. Journal of Computing & Information
Technology, 28(4), 269–285.
National Association of Insurance Commissioners. (2021). Insurance Fraud. Retrieved from https://content.naic.org/cipr_topics/topic_insurance_fraud.htm
National Conference of State Legislatures (2022). Medicaid. https://www.ncsl.org/research/health/medicaid-home-page.aspx
National Health Care Anti-Fraud Association (2019) The Challenge of Health Care Fraud. https://www.nhcaa.org/tools-insights/about-health-care-fraud/the-challenge-of-health-care-fraud/
Palmer, J. (2021) 35 Workers’ Compensation Statistics Every Pro Should Know. Breeze. https://www.meetbreeze.com/blog/workers-compensation-statistics/
Prince, A. E. R. (2016). Tantamount to Fraud?: Exploring Non-Disclosure of Genetic Information in Life Insurance Applications as Grounds for Policy Rescission. Health Matrix (Cleveland,
Ohio : 1991), 26, 255–307.
Reinsurance Group of America. (2019 December 14). Don’t Ignore Fraud’s Red Flags: The Key to Fighting Fraud is Preventing it. Retrieved on October 25, 2021, from
https://www.rgare.com/knowledge-center/media/articles/don't-ignore-fraud's-red-flags-the-key-to-fighting-fraud-is-preventing-it
Reinsurance Group of America. (2017). Global Claims Fraud Study. https://www.rgare.com/docs/default-source/knowledge-center-articles/rga-2017-global-claims-fraud-survey-white-paper-
--final.pdf?sfvrsn=601a588_0
Reinsurance Group of America. (2017). Investigating Life Insurance Fraud and Abuse. https://www.rgare.com/knowledge-center/media/research/investigating-life-insurance-fraud-and-abuse
Reinsurance Group of America. (2017). Global Claims Fraud Survey. rga-2017-global-claims-fraud-survey-white-paper---final (1).pdf
Rukhsar, L., Bangyal, W. H., Nisar, K., & Nisar, S. (2022). Prediction of Insurance Fraud Detection using Machine Learning Algorithms. Mehran University Research Journal of Engineering and
Technology, 41(1), 33. https://doi.org/10.22581/muet1982.2201.04
Sen, P. (2020). Life Insurance Frauds. Journal of the Insurance Institute of India, 8(1), 53–56.
Shah, D., Asthana, K., (2018). Life Insurance Fraud–Risk Management and Fraud Prevention. International Journal of Marketing, Financial Services & Management Research, 2(5).
Skiba, J.M. (2017). Psychology of Fraud. iUniverse, Bloomington, IN.
Social Security Administration. (2020). Annual Performance Report Fiscal Year 2020. OIG Mgmt Challenges (4).pdf
Social Security Administration. (2021) Inspector General Statement on the Social Security Administration’s Major Management and Performance Challenges.
https://www.ssa.gov/finance/2021/Inspector%20General%20Statement%20on%20the%20Social%20Security%20Administration's%20Major%20Management%20and%20Performance%2
0Challenges.pdf
Social Security Administration. (2022). Overview of our Disability Programs. https://www.ssa.gov/redbook/eng/overview-disability.htm?tl=0%2C1
Statista. 2021. https://www.statista.com/statistics/407741/gross-premiums-written-by-us-property-and-casualty-insurance/
Subudhi, S., & Panigrahi, S. (2020). Use of optimized Fuzzy C-Means clustering and supervised classifiers for automobile insurance fraud detection. Journal of King Saud University:
Computer and Information Sciences, 32(5), 568. https://doi.org/10.1016/j.jksuci.2017.09.010
Texas Department of Insurance. (2022). https://www.tdi.texas.gov/wc/index.html
United States Census Bureau. (2020). Health Insurance Coverage in the United States: 2019. https://www.census.gov/library/publications/2020/demo/p60-
271.html#:~:text=The%20percentage%20of%20people%20with,of%202019%20was%2092.0%20percent.&text=Private%20health%20insurance%20coverage%20was,point%20during%2
0the%20year%2C%20respectively.
United States Government Accountability Office. (2019). Congressional Address. MEDICARE AND MEDICAID CMS Should Assess Documentation Necessary to Identify Improper Payments.
https://www.gao.gov/assets/gao-19-277.pdf
University of Southern California. (2021). Medicare Fraud, Errors, and Abuse Can Cost in Dollars and Health. https://eldermistreatment.usc.edu/medicare-fraud-errors-and-abuse-can-cost-
in-dollars-and-health/#:~:text=Medicare%20loses%20approximately%20%2460%20billion,of%20a%20misunderstanding%20about%20benefits.
Verisk. (2017) Auto Insurance Premium Leakage: A $29B Problem for the Industry. https://www.verisk.com/insurance/visualize/auto-insurance-premium-leakage-a-29b-problem-for-the-
industry/#:~:text=According%20to%20Verisk%20estimates%2C%20personal,that%20undermines%20their%20rating%20plans.
Yan, C., Li, M., Liu, W., & Qi, M. (2020). Improved adaptive genetic algorithm for the vehicle Insurance Fraud Identification Model based on a BP Neural Network. Theoretical Computer
Science, 817, 12. https://doi.org/10.1016/j.tcs.2019.06.025
PHOTOS:
https://www.iii.org/fact-statistic/facts-statistics-workplace-safety-workers-comp
https://www.iii.org/article/background-on-insurance-fraud
rga-2017-global-claims-fraud-survey-white-paper---final (1).pdf
https://www.verisk.com/insurance/visualize/auto-insurance-premium-leakage-a-29b-problem-for-the-industry/

ACKNOWLEDGEMENTS
Technical review and oversight of the this report were provided by
the Coalition’s Research Committee:
David Rioux, Erie Insurance
Steven R. Jarrett, Westfield Group
Steve Friedman, Liberty Mutual Insurance
Timothy Hopper, Sentry Insurance
Pranay Mittal, Travelers Insurance
Junius Nottingham, Blue Cross Blue Shield Association
Steve Piper, CNA Insurance
Joseph Theobald, Citizens Property Insurance Corporation
The Coalition Against Insurance Fraud is America’s only anti-fraud
alliance speaking for consumers, insurance companies, government
agencies and others. Through its unique work, the Coalition
empowers consumers to fight back, helps fraud fighters to better
detect this crime and deters more people from committing fraud.
The Coalition supports this mission with a large and continually
expanding armory of practical tools: Information, research and data,
services, and insight, as a leading voice in the anti-fraud community.
Formed in 1993, the Coalition is made up of more than 260 member
organizations and they unite to fight all forms of insurance scams
regardless of who commits the fraud.
About the Coalition
C O N T A C T
Coalition Against Insurance Fraud
1012 14th Street NW, Suite 1105
Washington, DC 20005
202-393-7330 | [email protected]
